Learning Objectives
After completing this knowledge-based continuing education activity, pharmacists and pharmacy technicians will be able to
- DIFFERENTIATE between perimenopause and menopause
- DISCUSS the age-related loss of estrogen and its relation to symptoms of perimenopause and menopause
- IDENTIFY remedies and lifestyle adjustments for perimenopause and menopause
Release Date:
Release Date: August 15, 2025
Expiration Date: August 15, 2028
Course Fee
Pharmacists: $7
Pharmacy Technicians: $4
ACPE UANs
Pharmacist: 0009-0000-25-051-H01-P
Pharmacy Technician: 0009-0000-25-051-H01-T
Session Codes
Pharmacist: 25YC51-SLP74
Pharmacy Technician: 25YC51-LPS47
Accreditation Hours
2.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-25-051-H01-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
| Yvonne Riley-Poku |
| PharmD, RPh |
| Medical writer |
| Storrs, CT |
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Yvonne Riley-Poku, PharmD, RPh, has no relationships with ineligible companies and therefore have nothing to disclose.
ABSTRACT
Awareness about menopause is growing. It is now common to see menopause information on social media platforms and national news outlets. Menopause, sometimes referred to as “the change of life,” is a natural part of biological aging in women. Every woman who lives long enough will experience menopause, but its arrival affects some women physically, mentally, and emotionally. Menopausal hormone replacement therapy (HRT) is an option for treatment of certain symptoms, but it comes with risks. The U.S. Food and Drug Administration (FDA) has specific approved indications for HRT and various organizations such as the United States Preventive Task Force and the Menopause Society have issued their positions and recommendations for its use. Non-hormonal therapies are available, and lifestyle modifications may also help offset some health risks that are associated with this stage in a woman’s life.
CONTENT
Content
INTRODUCTION
Menopause is a natural part of biological aging in women. This phenomenon marks the end of reproductive years, and every woman who lives long enough will experience it.1 Often beginning in perimenopause—the period of time leading up to menopause—women experience many symptoms and health risks.1,2
Approximately 1.3 million women in the United States (U.S.) enter menopause every year.3 Despite being a natural result of aging, menopause has historically been shrouded in secrecy and seldom openly discussed, but the New York Times reports that high profile women and female celebrities alike are now openly discussing their experience with menopause. It also reports that the market is being flooded with menopause-related beauty products and telemedicine start-ups.4
With increased interest, a growing movement to increase awareness, and information flooding the Internet, it is important now more than ever for women to receive accurate information from healthcare providers and reputable sources. However, a recent survey revealed that nationally, most obstetrics and gynecology residency programs lack a dedicated menopause curriculum. Most program directors also agreed that their programs needed more menopause education resources.5
Many symptoms and health risks of menopause, if left unmanaged, have an impact on a woman’s quality of life, productivity, and emotional state. Women are living longer, and a woman may live many years after menopause. Globally, a woman aged 60 years in 2019 could expect to live on average another 21 years.1
Years after the National Institutes of Health's (NIHs) Women's Health Initiative, HRT as an option for certain symptoms in postmenopausal women is back in the spotlight. Now, physicians take a nuanced approach to HRT, considering certain individual patient factors.6,7
It is important for women to recognize symptoms, understand the risk of chronic conditions, and generally educate themselves about the menopause transition. Being well-informed about the menopause transition means women can be proactive and lead healthier lifestyles to counter the issues that may arise with menopause such as bone loss and cardiovascular disease. Proper management during this period results in healthy aging and better quality of life. Menopause is a universal female experience, and it is vital that both physicians and women alike be appropriately informed about it.
PAUSE AND PONDER: What do you wish you knew about menopause before you or a loved one began the menopause transition?
DEFINING MENOPAUSE AND ITS EFFECTS
Perimenopause is the period leading up to menopause and signals the final years of a woman’s reproductive life. This period can last several years, the average being four years.2 It begins with irregular menstrual cycles marked by a gradual loss of ovarian follicular function (i.e., ovaries begin to stop releasing eggs for fertilization) and a decline in circulating estrogen and progesterone levels.1,2 This period may usher in a slew of symptoms, and the hormonal changes and fluctuations are often responsible for them.2 A woman can still get pregnant during perimenopause because although menstruation is irregular, the ovaries can still release eggs for fertilization. It is impossible to accurately predict ovulation, and women must use adequate birth control until one full year after the last period to avoid unwanted pregnancy.2
Menopause marks the end of the reproductive years for women.1,2 Menopause occurs or is diagnosed after 12 consecutive months without menstruation in the absence of clinical intervention or other physiologic or pathologic cause.1 This means that a woman could go 11 months with no menstruation and then have a period in the 12th month. The clock would then begin all over again. A woman cannot become naturally pregnant after menopause because the ovaries have stopped releasing eggs for fertilization. Importantly, they can still contract sexually transmitted diseases, so experts advise women to use adequate protective measures.2
The average age of menopause in the U.S. is 52.2 Genetics, lifestyle, and environmental factors influence the age at menopause and the timing of symptoms throughout the menopausal transition. According to the World Health Organization, for women worldwide, natural menopause generally occurs between age 45 and 55.1 The SIDEBAR lists factors that trigger early menopause.
SIDEBAR: Factors That Trigger an Early Onset of Menopause1,2
- Surgical procedures that involve removing both ovaries
- Medical interventions that cause termination of ovarian function, such as radiation therapy and chemotherapy
- Premature menopause, or menopause before age 40 due to chromosomal abnormalities, autoimmune disorders, or other unknown causes
Menopausal Hormone Changes
Years before menopause occurs, ovarian function begins to fluctuate.2 This is a progressive process often responsible for many of the symptoms women experience during this period.
How this Happens
Ovaries are the primary estrogen source in a woman’s body, with follicles synthesizing and releasing the hormone. An ovary has the greatest number of oocytes (about 1 to 2 million) at birth. Oocytes are the immature cells within a follicle that potentially mature into fully developed eggs. A fully developed egg is released from the ovary during ovulation and travels down the fallopian tube to be potentially fertilized.8,9
As women age, the number of follicles in their ovaries decrease. During a physiological process known as atresia, ovarian follicles that contain oocytes degenerate and die. This is a normal process that happens in all women. The process ensures that only healthy follicles with oocytes mature and ovulate. During atresia, follicle cells die, eggs break down, and macrophages and other follicular cells resorb the follicle contents. Although ovulation will also decrease the number of follicles, the vast number of follicles are decreased through atresia. At some point the number of follicles and oocytes reach critically low levels in the ovaries. Since these are responsible for producing estrogen, this is when women begin to experience symptoms associated with estrogen depletion.8,9
At various stages during the menopause transition, women may only have a few hundred to a few thousand oocytes left. Estrogen levels decrease and menstrual periods become irregular. As various tissues in the body have estrogen receptors, when estrogen levels decrease or fluctuate, several systems can develop and women experience many of the symptoms of perimenopause and menopause.8,9
Progesterone levels also decrease during the menopausal transition. After ovulation releases the egg from the follicle, the leftover contents of the empty follicle form the corpus luteum, a temporary gland that produces progesterone.10 Progesterone thickens the endometrium (lining of the uterus) for a fertilized egg to implant and grow. If pregnancy occurs, the placenta takes over the production of progesterone. In the absence of pregnancy, progesterone levels drop, causing the endometrium to shed (causing menstruation). During the menopause transition, the ovaries no longer produce high levels of estrogen and progesterone in the absence of regular ovulation.10
Symptoms of Menopause
Hormonal changes and fluctuations lead to the many symptoms associated with perimenopause and menopause, some more common than others and affecting each woman differently, with varying degrees of severity. Vasomotor symptoms (VMS) like hot flashes are the most recognized and reported symptom of menopause.11 Table 1 describes the symptoms a woman may experience during and after the menopause transition listed in the order in which they typically occur. For less common symptoms of menopause, see the SIDEBAR. Some women may be able to tolerate menopausal symptoms with lifestyle changes alone, while others may require hormonal remedies, non-hormonal remedies, or a combination of both.11
Table 1. Signs and Symptoms of Perimenopause and Menopause2,12-15
| Symptom | Description |
| Irregular periods
|
Starts the menopause transition
Unpredictable ovulation causes changes in menstrual cycle patterns Could be months of missed periods, varying lengths of time between cycles (longer or shorter), and menstrual flow changes |
| Vasomotor Symptoms ( hot flashes, night sweats)
|
This is a sudden feeling of heat in the face, neck, and chest that is often accompanied by flushing, perspiration, and acute feelings of physical discomfort. May be followed by cold shivering. This may last up to several minutes. Night sweats are hot flashes that cause sweating during sleep. Vasomotor symptoms can occur before, during, and after menopause. |
| Genitourinary symptoms | Symptoms include dysuria, urinary incontinence, increased urinary frequency, vaginal and cervical atrophy (thinning, drying, and inflammation of the vaginal walls), sexual dysfunction, and decreased libido. Vaginal dryness presents an increased risk for sexually transmitted diseases. |
| Weight gain | While weight gain occurs in both men and women with aging, a particular increased deposition of visceral and subcutaneous adipose tissue to the abdomen in women during the menopause transition occurs.
For weight gain before menopause, estrogen makes it possible for subcutaneous adipose tissue to deposit in the gluteal and femoral regions. After menopause this deposition moves to the abdominal region due to the decrease in estrogen levels. Abdominal fat distribution carries the risk of cardiovascular and metabolic diseases. |
| Sleep disruption | Sleep duration changes with advancing age, however during the menopause transition, concurrent changes in women’s reproductive hormone levels influence sleep duration and quality. It may be harder to fall asleep and stay asleep. Night sweats may also disrupt sleep. |
| Mood changes depression, anxiety | Estrogen receptors are in the brain including areas involved in mood regulation. Stress, work, and family responsibilities affect mood during this period. Although the exact mechanism is unknown, mood symptoms may additionally be related to fluctuating estrogen levels. Some women may feel irritable or have crying spells.
Depression and anxiety may be caused by fluctuating hormones, menopausal symptoms, or both. |
SIDEBAR: Less Common Symptoms of Menopause16
Experts are continually learning about menopause’s symptoms. Gradual estrogen loss may be responsible for these less common symptoms of menopause:
- Dry eye syndrome and vision changes
- Easier bruising due collagen changes in the skin
- Return of acne
- Joint pain and stiffness
- Growing rogue hairs on chin or cheeks
The menopause transition can cause a wide variety of symptoms, but other serious conditions can cause these too. It is always important to consult a provider to rule these out.
PAUSE AND PONDER: How many symptoms of perimenopause and menopause can you name aside from hot flashes?
Chronic Conditions and Long-Term Consequences
Long term complications of menopause are related to low estrogen levels. Two major complications of concern are cardiovascular disease and osteoporosis.
Declining estrogen in menopause increases the risk of cardiovascular disease.2 Coronary heart disease rates are two to three times higher in those who have reached menopause than those at the same age who have not. Women generally have a lower risk of heart disease than men before the age of 55, but after menopause, women reach the same level of risk for heart disease as men of the same age.2
Estrogen deficiency during menopause also causes the typical bone loss or decreased bone density seen in osteoporosis.2 Up to 20% of bone loss can happen during this period.17 The consequences of osteoporosis are an increased risk of fractures, pain, mobility issues, and loss of height. Osteoporosis, a progressive condition, can worsen over time.
Menopause symptoms also adversely affect women in the workplace. Middle aged women contribute greatly to the global workforce and could potentially face increased health care costs and lost opportunities for career advancement. Mayo Clinic conducted a study to determine the estimated economic impact of menopause symptoms based on missed days from work; hours cut back at work; and quitting, retiring, or changing jobs. Based on missed workdays alone, these researchers estimated an annual loss of $1.8 billion in the U.S. due to menopause-related symptoms.18
MENOPAUSAL HORMONE REPLACEMENT THERAPY
The Ongoing Debate of HRT
Experts have debated menopausal HRT use for decades. Studies in the mid-1970s showed that women who used estrogen alone had an increased risk of endometrial cancer.19,20 Researchers found that adding progesterone to estrogen provided protection against uterine cancer. Since then, progesterone is added to hormone treatment for women who have an intact uterus.7,19,20
Between 1993 and 1998, the NIH began The Women’s Health Initiative, to study strategies to prevent and control some of the most common causes of morbidity and mortality in postmenopausal women (e.g., cardiovascular disease, osteoporosis, cancer).21 Researchers randomized more than 27,000 postmenopausal women aged 50 to 79 in the HRT portion of the trial. Those with a uterus (n = 16,608) received either combined conjugated equine estrogen (CEE 0.625 mg/day) plus medroxyprogesterone acetate (MPA 2.5 mg/day) or placebo. Women without a uterus (i.e., prior hysterectomies) were assigned to CEE alone or placebo.22,23 The primary outcome was coronary heart disease incidence, and the primary safety outcome was invasive breast cancer incidence. To summarize overall effects, researchers also looked at other risks and benefits of HRT in addition to the primary outcomes. These included colorectal cancer, hip fracture, and cardiovascular risks.22,23
After about five years, results began to show that the risks of HRT outweighed the benefits. HRT was associated with an increased risk of stroke, heart disease, and breast cancer. However, the results also indicated a reduction in osteoporotic fractures and colorectal cancers but no significant cardiovascular benefits. Ultimately, the research team stopped the trial early. Many physicians stopped prescribing HRT, and many women abandoned it altogether.6,7
Despite stopping the trial, researchers continued to follow up with trial participants until 2010.24,25 They reanalyzed the data based on results from the intervention, post-intervention, and follow-up phases with consideration for the trial participants’ ages. Researchers concluded that the trial findings do not support HRT for chronic disease prevention. They have since noted that HRT may be beneficial for bothersome symptoms among women in early menopause (i.e., women 50 to 59 years of age) or within 10 years of menopause onset. Data do not support HRT for chronic disease prevention in this subset either. These women must have no contraindications and must be interested in taking HRT.24,25
Extensive debate continues, but several groups such as the U.S. Preventive Service Task Force (USPSTF) and the Menopause Society, have published position statements and recommendations for HRT use. The USPSTF is an independent panel of experts in disease prevention and evidence-based medicine that makes recommendations about clinical preventive services. The Menopause Society, formerly known as the North American Menopause Society, is a non-profit organization dedicated to improving women’s health during menopause and beyond, by providing resources for both healthcare professionals and the public.
Several organizations have issued recommendations on HRT use in postmenopausal individuals, particularly regarding its benefits, risks, and approved indications. While the general consensus is that HRT is the most effective treatment for VMS and genitourinary syndrome of menopause, its role in preventing chronic conditions such as osteoporosis remains controversial. The U.S. Food and Drug Administration (FDA) and the Menopause Society support HRT for VMS, genitourinary symptom management, and osteoporosis prevention in appropriate candidates, especially women younger than age 60 or within 10 years of menopause onset. In contrast, USPSTF recommends against using HRT solely for the primary prevention of chronic conditions in asymptomatic individuals. Recommendations emphasize shared decision-making and individual risk assessment.26-28
Forms of Hormone Therapy
Menopausal HRT involves the administration of synthetic estrogen and progesterone to replace a woman’s hormone levels to help alleviate symptoms. Women should be educated on the risks and benefits of HRT, consider their personal risk, and be willing to take HRT, before starting treatment.26-28
The current recommendations are for postmenopausal women younger than 60 years or women who are within 10 years of menopause onset and have no contraindications. These women must also be willing to take HRT.26-28 HRT use is not recommended in women after the age of 60, or in those who are 10 years post menopause. The FDA has approved HRT for VMS, urogenital symptoms, and postmenopausal osteoporosis prevention.
HRT may be given as estrogen alone, progestin alone, or a combination estrogen and progestin. The FDA has approved several formulations, including oral, topical, transdermal, and injectable dosage forms.29 Table 2 lists FDA-approved HRT products.
Women with an intact uterus with no other contraindications or risks who are willing to take HRT for menopause may receive estrogen in combination with progesterone. Estrogen therapy alone causes the endometrial lining to grow unopposed. Adding progesterone to the regimen prevents this abnormal growth and thus reduces risk of malignancy.19,20
Women with no other contraindications or risks who have had a hysterectomy and are willing to take HRT may receive estrogen therapy alone. In such cases, progesterone is unnecessary.19,20
Table 2. FDA-Approved Hormone Replacement Therapies29
| Generic Name | How Supplied | Brand Name(s) |
| Estrogen-Only | ||
| Conjugated estrogens | Oral | Premarin |
| Vaginal cream | Premarin | |
| Injection | Premarin | |
| Estradiol | Gel | Divigel, Elestrin, Estrogel |
| Transdermal patch | Alora, Climara, Menostar*, Minivelle, Vivelle, Vivelle-Dot | |
| Transdermal skin spray | Evamist | |
| Vaginal cream | Estrace | |
| Vaginal ring | Estring | |
| Vaginal tablet | Vagifem | |
| Estradiol acetate | Vaginal ring | Femring |
| Estradiol valerate | Injection | Delestrogen |
| Estropipate | Oral | Ogen |
| Progestin-Only | ||
| Medroxyprogesterone acetate | Oral | Provera |
| Micronized progesterone | Oral | Prometrium |
| Combination Therapies | ||
| Conjugated estrogen/ bazedoxifene** | Oral | Duavee |
| Conjugated estrogen/ medroxyprogesterone | Oral | Prempro |
| Estradiol/drospirenone | Oral | Angeliq |
| Estradiol/levonorgestrel | Transdermal patch | Climara Pro |
| Estradiol/norethindrone acetate | Oral | Activella |
| Transdermal patch | Combipatch | |
| Norethindrone acetate/ethinyl estradiol | Oral | Femhrt |
*Menostar is for osteoporosis prevention only. **Bazedoxifene is not a hormonal therapy.
Due to the known risks of menopausal HRT use, all patients need a thorough evaluation—including a detailed medical history and physical examination—for a proper diagnosis and to identify potential contraindications. Providers and patients must also assess whether the benefits outweigh the risks on an individualized basis. Women should use HRT at the lowest possible dose and for the shortest possible duration to achieve symptomatic relief while avoiding adverse effects.30
Women should not take HRT if they have29
- problems with vaginal bleeding
- current or past cancers, such as breast cancer or uterine cancer
- current or past blood clot, stroke, or heart attack
- bleeding disorders
- liver disease
- allergy to hormone medicine
NON-HORMONAL THERAPIES FOR MENOPAUSE
Risks of menopausal HRT outweigh its benefits for many patients, so additional options are needed. The FDA has approved a few non-hormonal options for women who are ineligible for or uninterested in HRT, and others many opt to use off-label or complementary and alternative medicines.26
FDA-Approved Therapies
Fezolinetant
The FDA recently approved an oral medication fezolinetant (Veozah) for the treatment of moderate to severe VMS caused by menopause. Fezolinetant is a neurokinin-3 (NK3) receptor antagonist that binds to and blocks the activities of the neurokinin-3 receptor, which plays a role in the brain’s regulation of body temperature.31
Fezolinetant is supplied as a 45 mg tablet, taken once daily with or without food. It has been associated with a risk of elevated hepatic transaminases, leading the FDA to add a Boxed Warning about the risk of liver injury more than a year after initial approval.32 Blood work to check for liver damage is required before fezolinetant use and every three months for the first nine months after initiation of therapy.31
Adverse effects of fezolinetant include abdominal pain, diarrhea, insomnia, back pain, hot flush, and elevated hepatic transaminases. Symptoms relating to liver damage to watch for include nausea, vomiting, and yellowing of the skin and eyes. Patients experiencing these must consult their prescriber immediately. Fezolinetant is contraindicated in patients with cirrhosis, severe renal damage, or end-stage renal disease.31
Paroxetine
Paroxetine (Brisdelle) is a selective serotonin reuptake inhibitor (SSRI) FDA-approved for the treatment of moderate to severe VMS. It is not an estrogen and its mechanism of action for the treatment of VMS is unknown.33 The recommended dose is one 7.5 mg capsule daily at bedtime with or without food. This medication contains a lower dose of paroxetine than those used for other indications (e.g., depression, obsessive compulsive disorder) and is not approved for any psychiatric conditions.
Paroxetine’s common adverse effects include headache, fatigue, and nausea and vomiting. Paroxetine has a Boxed Warning for the potential of increased risk of suicidal thoughts and behaviors, and serotonin syndrome. The FDA warns prescribers to monitor for worsening and emergence of these severe symptoms. Contraindications include concomitant use or within 14 days of monoamine oxidase inhibitors, use with thioridazine or pimozide, hypersensitivity to any ingredient, and pregnancy. VMS do not occur during pregnancy and paroxetine may cause fetal harm.33
Selective Estrogen Receptor Modulators
Raloxifene and ospemifene are selective estrogen receptor modulators (SERMs) FDA-approved for varying uses during menopause. Bazedoxifene is another FDA-approved SERM, which is found only in a combination tablet with conjugated estrogens.
Raloxifene (Evista) is SERM indicated for treatment and prevention of osteoporosis in post-menopausal women.34 Patients take one 60 mg tablet once daily. Common adverse effects include hot flashes, leg cramps, peripheral edema, flu syndrome, arthralgia, and sweating.34 Raloxifene is contraindicated in women with active or history of venous thromboembolism, including deep vein thrombosis, pulmonary embolism, and retinal vein thrombosis. It is also contraindicated for use in pregnancy, as it may cause fetal harm.34 The FDA’s Boxed Warning cautions of an increased risk of venous thromboembolism and death from stroke. Providers must consider the risk-benefit balance in women at risk for stroke. Concomitant use is not recommended or caution should be used when raloxifene is taken with cholestyramine, warfarin, and other highly protein-bound drugs (e.g., diazepam, diazoxide, lidocaine).34
Ospemifene (Osphena) is a SERM indicated for the treatment of moderate to severe vaginal dryness and dyspareunia due to menopause.35 Patients take one 60 mg oral tablet once daily with food. Ospemifene acts just like estrogen in some parts of the body but not in others. 35 It has estrogen agonistic effects on the endometrium, which has led the FDA to add a Boxed Warning of a risk of endometrial cancer. With its estrogen agonist/antagonist profile, the FDA has another Boxed Warning of an increased risk of cardiovascular disorders (stroke, coronary heart disease, venous thromboembolism). 35 Ospemifene should be used for the shortest duration consistent with treatment goals and risks for the individual woman.35 Common adverse effects include hot flush, vaginal discharge, muscle spasms, headache, hyperhidrosis, vaginal hemorrhage, and night sweats. Contraindications to ospemifene use include35
- undiagnosed abnormal genital bleeding
- estrogen-dependent neoplasia
- hypersensitivity to ospemifene
- active or history of deep vein thrombosis or pulmonary embolism
- active or history of arterial thromboembolic disease (e.g., stroke, myocardial infarction)
Women taking ospemifene should not take estrogen or estrogen agonist/antagonists, fluconazole, or rifampin concomitantly.35
Bazedoxifene is a SERM available in combination with conjugated estrogens (Dauvee) indicated for the treatment of moderate to severe VMS and postmenopausal osteoporosis prevention in women with a uterus. Bazedoxefine acts as an estrogen agonist in some estrogen-sensitive tissues and as an antagonist in others (e.g., the uterus). The pairing of conjugated estrogens with bazedoxifene produces a composite effect that is specific to each target tissue. The bazedoxifene component reduces the risk of endometrial hyperplasia that can occur with the conjugated estrogens component. Patients take one tablet (conjugated estrogens/bazedoxifene 0.45 mg/20 mg)daily with or without food for both indications.36
Women taking conjugated estrogens/bazedoxifene should add supplemental calcium and/or vitamin D to their diets if intake is inadequate.
Contraindications to conjugated estrogens/bazedoxifene include36
- Undiagnosed abnormal uterine bleeding
- Known, suspected, or a history of breast cancer
- Known or suspected estrogen-dependent neoplasia
- Active or history of deep vein thrombosis and pulmonary embolism
- Active or history of arterial thromboembolic disease (stroke, myocardial infarction)
- Known hepatic impairment or disease
- Hypersensitivity to estrogens, bazedoxifene or any ingredients
- Known protein C, protein S, or antithrombin deficiency or other known thrombophilic disorders
- Pregnancy
Women taking conjugated estrogens/bazedoxifene should not take progestins, additional estrogens, or additional estrogen agonists/antagonists.
Adverse reactions include a risk for malignant neoplasms (endometrial cancer, breast cancer, ovarian cancer), cardiovascular disorders (stroke, coronary heart disease, venous thromboembolism), gallbladder disease and hypertriglyceridemia.36
Off-Label Therapies
In 2023, The Menopause Society conducted an evidence-based review of the most current and available literature to determine whether to recommend some management options for menopause associated VMS. They recommended some SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), and gabapentin.37
Researchers have found in large randomized, double-blind, placebo-controlled trials that paroxetine, citalopram, escitalopram, venlafaxine, desvenlafaxine, and duloxetine reduce hot flashes by 24% to 69%. These medications are also first-line therapies for mood disorders such as depression and anxiety. For women with new onset or worsening mood disorders, which are common in menopause, these medications may be beneficial.38,37 Common adverse effects associated with use of SSRIs and SNRIs include nausea, weight gain, gastrointestinal disorders, headache, and sexual dysfunction. Lower doses are generally used for VMS rather than the higher doses used for mood disorders.38
In very small randomized double-blind, placebo-controlled trials, gabapentin was effective at reducing hot flash frequency by 45% to 51% compared to placebo.39,40 It was also shown to be a well-tolerated treatment for hot flashes.40 Gabapentin is also used as treatment for neuropathic pain and epilepsy and may help with sleep when taken at bedtime. Adverse effects include dizziness and coordination difficulties, weight gain, edema, and lethargy. Patients should use the lowest effective dose to minimize these negative adverse effects.38
Complementary and Alternative Medicine
Some complementary and alternative medicines (CAMs) make claims about easing menopausal symptoms. Complementary health approaches to menopause may include any or all of the following41:
- nutritional (e.g., dietary supplements, special diets)
- psychological (e.g., meditation, hypnosis, relaxation therapies)
- physical (e.g., massage therapy, acupuncture)
- combination approaches (e.g., yoga, tai chi [physical and psychological])
CAMs are not regulated the same way as FDA-approved medications. Although some dietary supplements have been studied for menopause symptoms, none have been shown to be clearly helpful. Little information is available on long term safety of dietary supplements for menopause and some supplements may have harmful adverse effects or drug interactions.
In 2023, the Menopause Society released its position statement on non-hormonal approaches for menopause-related VMS based on an evidence-based review of current literature.37 For CAM, it recommended cognitive behavioral therapy and clinical hypnosis as options for the treatment of VMS. The Menopause Society did not recommend yoga, acupuncture, or any natural products for VMS.37
According to the NIH’s National Center for Complementary and Integrative Health, the evidence has not clearly shown that phytoestrogens, herbs, and other dietary supplements; acupuncture; or yoga relieve menopause symptoms.41
Phytoestrogens are substances from plants that have chemical structures similar to those of estrogen. Flaxseed is a phytoestrogen source and the isoflavones found in soy and red clover are also phytoestrogens. Studies on their ability to relieve menopause symptoms have been inconsistent, or no more effective than placebo. Phytoestrogens may be safe for short term use, but their long-term safety has not been established and may not be safe for women who should not take estrogen.41
Regarding custom-mixed (compounded) bioidentical hormones, the group reports that the evidence does not support claims that they are more effective than conventional HRT. They also warn that compounded bioidentical hormones have not been shown to be safer than other forms of HRT, and that their content may vary from batch to batch.41
PAUSE AND PONDER: In what ways have you made or supported a loved one in making lifestyle changes to adequately prepare for “the change of life?”
Lifestyle Modification During and After Menopause,
To stay healthy during and after menopause, lifestyle changes and modifications (illustrated in Figure 1) are beneficial. Lifestyle changes and modifications may make menopausal symptoms bearable even if symptoms are not completely eliminated. Lifestyle changes may also help prevent the chronic conditions of menopause such as cardiovascular disease, osteoporosis, and insulin resistance. It may also help with mood and sleep and help prepare a woman for healthy aging.42
Figure 1. Lifestyle Modifications for During and After Menopause 43
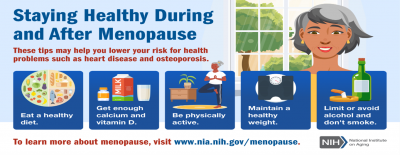
At least 30 minutes of physical activity on most days of the week helps women maintain a healthy weight and is good for the bones, heart, and mood. Women should aim for a mix of moderate and vigorous aerobic activities and exercises that build muscle strength, such as weight-bearing exercises.42,44 Women should obtain advice from their healthcare provider before beginning any physical activity.
Eating a healthy diet can help counter some of the symptoms women experience in the menopause transition and prevent chronic illnesses and certain cancers. Essential nutrients to focus on in menopause include vitamins B, C, D, calcium, and protein for energy. A healthy diet also helps with the maintenance of a healthy weight, which improves cholesterol levels, reduces the risk for diabetes, improves blood pressure, and improves daily function.42,44
Good sleep is essential for health and emotional well-being. Insufficient sleep duration and quality may be a problem during this period in a woman’s life. Hot flashes and night sweats are also disruptive to sleep. Getting enough sleep lowers the risks for chronic conditions such as high blood pressure, diabetes, and heart disease. It also improves attention and memory. Regular exercise, a healthy diet, avoiding caffeine and alcohol before bedtime, and going to bed and getting up at the same time each day can improve sleep.44
Cognitive function at midlife appears to be influenced by the stage of menopause and menopausal symptoms such as sleep difficulties and mood changes. Many life stressors cannot be altered, but coping skills and strategies are beneficial to maintain a balance between self-nurturing and the obligations of work and caring for others. To improve and maintain cognition and mood, women should consider maintaining a social network, remaining physically and mentally active, and following a healthy diet.44 Maintaining quality social contacts is beneficial during this period. Actively engaging with friends, family, and the community in positive ways helps improve health and emotional wellbeing.
Smoking is damaging to health in many ways. It causes heart disease, reduces bone density, and causes many forms of cancer. Experts advise women to stop smoking and limit alcohol consumption.42,44
CONCLUSION
Discussions about menopause are no longer taboo. While HRT is beneficial and remains an option for women with no risk factors and contraindications, it is not a one-size fits all solution. HRT comes with risks and providers must assess patients carefully before treatment initiation and consider patient preferences. Non-hormonal therapies are available for women who may be unable or unwilling to take HRT. Women are living longer, and a woman may live for several years post-menopause. Lifestyle changes and modifications help counter the chronic conditions that often arise post-menopause and are important and necessary for healthy aging in women.
Pharmacist Post Test (for viewing only)
Spotlight on Perimenopause and Menopause: What Pharmacy Teams Should Know
Pharmacist Post-test 25-051
After completing this continuing education activity, pharmacists will be able to
• DIFFERENTIATE between perimenopause and menopause
• DISCUSS the age-related loss of estrogen and its relation to symptoms of perimenopause and menopause
• IDENTIFY remedies and lifestyle adjustments for perimenopause and menopause
1. Which of the following is caused by the fluctuating hormone levels of perimenopause?
A. Immediate, permanent cessation of ovulation
B. Early onset menopause
C. Symptoms that signal the transition to menopause
2. AB is a 45-year-old woman who has been on the same birth control for 5 years. She is experiencing occasional night sweats, and she has noticed weight gain particularly in her abdominal region. She has not had a menstrual period in 6 months. What is AB most likely experiencing?
A. Menopause
B. Perimenopause
C. Adverse effects of birth control
3. Women naturally undergo a process where follicles containing oocytes degenerate and die ensuring that only healthy follicles with oocytes mature and ovulate. What is this process known as?
A. Perimenopause
B. Atresia
C. Pregnancy
4. BC is a 48-year-old woman with an intact uterus seeking a remedy for her bothersome vasomotor symptoms. Based on her medical history, labs, and risk assessment, her OBGYN determines she is a candidate for hormone replacement therapy and BC agrees. Which of these regimens is appropriate?
A. Estradiol/norethindrone acetate
B. Conjugated estrogen/bazedoxifene
C. Medroxyprogesterone acetate
5. MD is 48 years old with an intact uterus experiencing bothersome vasomotor symptoms. Her provider determines that she is a candidate for hormone therapy based on her medical history, labs, and a risk assessment. MD is very concerned about the risks associated with hormone therapy. Which of the following is the BEST response?
A. “As long as you use both estrogen and progesterone, the risks are minimal.”
B. “The gabapentin you already take for neuropathic pain should be enough.”
C. “Fezolinetant may be a better option for you, I can contact your doctor.”
6. Experts advise women to make lifestyle modifications for healthy aging after menopause. Which one of these is the BEST recommendation?
A. Isolating from others for peace of mind
B. Drinking one glass of wine nightly for relaxation
C. Improving the diet and incorporating exercise
7. KG is in perimenopause, and although she is still asymptomatic, she expresses concern about the health conditions some women face post-menopause. She requests menopausal hormone replacement therapy to prevent possible cardiovascular disease and Type 2 diabetes. Which of these is the MOST appropriate response?
A. Hormone therapy is not recommended to prevent these chronic conditions
B. It’s a good idea to start hormone therapy early before symptoms arise
C. Her provider should prescribe paroxetine as preventive therapy instead
8. Which of the following is the progressive loss of estrogen during the menopause transition responsible for?
A. Ensuring that only healthy follicles with oocytes mature and ovulate
B. Thickening the endometrial lining to prepare for cessation of menstruation
C. Unpredictable ovulation and changes in menstrual cycle patterns
9. When do women experience vasomotor symptoms?
A. Only during menopause
B. During perimenopause and menopause
C. Only during post-menopause
10. What strategies can women implement to lower the risk for chronic conditions associated with menopause, including heart disease and osteoporosis?
A. Request hormone therapy before they begin the menopause transition
B. Make lifestyle modifications that may help counter some future health risks
C. Do nothing, the risk of menopause complications is not that significant
Pharmacy Technician Post Test (for viewing only)
Spotlight on Perimenopause and Menopause: What Pharmacy Teams Should Know
Pharmacy Technician Post-test 25-051
After completing this continuing education activity, pharmacists will be able to
• DIFFERENTIATE between perimenopause and menopause
• DISCUSS the age-related loss of estrogen and its relation to symptoms of perimenopause and menopause
• IDENTIFY remedies and lifestyle adjustments for perimenopause and menopause
1. Which of the following is caused by the fluctuating hormone levels of perimenopause?
A. Immediate, permanent cessation of ovulation
B. Early onset menopause
C. Symptoms that signal the transition to menopause
2. AB is a 45-year-old woman who has been on the same birth control for 5 years. She is experiencing occasional night sweats, and she has noticed weight gain particularly in her abdominal region. She has not had a menstrual period in 6 months. What is AB most likely experiencing?
A. Menopause
B. Perimenopause
C. Adverse effects of birth control
3. Women naturally undergo a process where follicles containing oocytes degenerate and die ensuring that only healthy follicles with oocytes mature and ovulate. What is this process known as?
A. Perimenopause
B. Atresia
C. Pregnancy
4. BC is a 48-year-old woman seeking a remedy for her bothersome vasomotor symptoms. She presents a prescription to the pharmacy for fezolinetant 60 mg tablet to be taken once daily. Why should you bring this to the pharmacist’s attention?
A. Fezolinetant is a 45 mg tablet
B. Fezolinetant is a suspension
C. Fezolinetant is not FDA-approved
5. MD is 48 years old and experiencing bothersome vasomotor symptoms. Her provider determines that she is a candidate for hormone therapy based on her medical history, labs, and a risk assessment. MD is very concerned about the risks associated with hormone therapy. Which of the following is a non-hormonal option to consider for MD?
A. Bazedoxifene
B. Estradiol vaginal ring
C. Fezolinetant
6. Experts advise women to make lifestyle modifications for healthy aging after menopause. Which one of these is the BEST recommendation?
A. Isolating from others for peace of mind
B. Drinking one glass of wine nightly for relaxation
C. Improving the diet and incorporating exercise
7. KG presents a prescription to the pharmacy for paroxetine 20 mg tablets. She mentions that it has been prescribed for her hot flashes. Why should you bring this to the pharmacist’s attention?
A. Paroxetine cannot be prescribed for hot flashes
B. Paroxetine dosing for hot flashes is 7.5 mg daily
C. Paroxetine 20 mg has been discontinued
8. Which of the following is the progressive loss of estrogen during the menopause transition responsible for?
A. Ensuring that only healthy follicles with oocytes mature and ovulate
B. Thickening the endometrial lining to prepare for cessation of menstruation
C. Unpredictable ovulation and changes in menstrual cycle patterns
9. When do women experience vasomotor symptoms?
A. Only during menopause
B. During perimenopause and menopause
C. Only during post-menopause
10. What strategies can women implement to lower the risk for chronic conditions associated with menopause, including heart disease and osteoporosis?
A. Request hormone therapy before they begin the menopause transition
B. Make lifestyle modifications that may help counter some future health risks
C. Do nothing, the risk of menopause complications is not that significant
References
Full List of References
1. World Health Organization. Menopause. October 16, 2024. Accessed April 10, 2025. https://www.who.int/news-room/fact-sheets/detail/menopause
2. U.S. Department of Health and Human Services. Office on Women’s Health. Menopause Basics. March 17, 2025. Accessed April 10, 2025. https://womenshealth.gov/menopause/menopause-basics
3. Society for women’s health research. Menopause. Accessed July 9, 2025. https://swhr.org/health_focus_area/menopause/
4. Larocca A. Welcome to the menopause gold rush. The New York Times. December 20, 2022. Accessed April 10, 2025. https://www.nytimes.com/2022/12/20/style/menopause-womens-health-goop.html
5. Allen JT, Laks S, Zahler-Miller C, et al. Needs assessment of menopause education in United States obstetrics and gynecology residency training programs. Menopause. 2023;30(10):1002-1005. doi:10.1097/GME.0000000000002234
6. Lobo RA. Hormone-replacement therapy: current thinking. Nat Rev Endocrinol. 2017;13(4):220-231. doi: 10.1038/nrendo.2016.164\
7. Cagnacci A, Venier M. The controversial history of hormone replacement therapy. Medicina (Kaunas). 2019;55(9):602. doi: 10.3390/medicina55090602.
8. Vollenhoven B, Hunt S. Ovarian ageing and the impact on female fertility. F1000Res. 2018;7:F1000 Faculty Rev-1835. doi: 10.12688/f1000research.16509.1
9. Zhou J, Peng X, Mei, S. Autophagy in Ovarian follicular development and Atresia. Int J Biol Sci. 2019;15(4):726-737. doi: 10.7150/ijbs.30369
10. Cleveland Clinic. Progesterone. December 29, 2022. Accessed April 10, 2025. https://my.clevelandclinic.org/health/body/24562-progesterone
11. The Menopause Society. Menopause Topics: Symptoms. Accessed April 10, 2025. https://menopause.org/patient-education/menopause-topics/symptoms
12. National Institute on Aging. What is menopause? October 16, 2024. Accessed April 10, 2025. https://www.nia.nih.gov/health/menopause/what-menopause
13. Knight MG, Anekwe C, Washington K, Akam EY, Wang E, Stanford FC. Weight regulation in menopause. Menopause. 2021;28(8):960-965. doi: 10.1097/GME.0000000000001792
14. Vahratian A. Sleep duration and quality among women aged 40–59, by menopausal status. NCHS data brief, no 286. Hyattsville, MD: National Center for Health Statistics. 2017. Accessed April 10, 2025. https://www.cdc.gov/nchs/data/databriefs/db286.pdf
15. The Menopause Society. Menopause Topics: Mental Health. Accessed April 10, 2025. https://menopause.org/patient-education/menopause-topics/mental-health
16. Mayo Clinic Press. Could this be menopause? Exploring lesser-known symptoms and what to do about them. April 23, 2024. Accessed April 10, 2025. https://mcpress.mayoclinic.org/menopause/could-this-be-menopause-exploring-lesser-known-symptoms-and-what-to-do-about-them/
17. Endocrine Society. Menopause and Bone Loss. January 24, 2022. Accessed July 14, 2025. endocrine.org/patient-engagement/endocrine-library/menopause-and-bone-loss
18. Faubion SS, Enders F, Hedges MS, et al. Impact of Menopause Symptoms on Women in the Workplace. Mayo Clin Proc. 2023;98(6):833-845. doi:10.1016/j.mayocp.2023.02.025
19. Woodruff JD, Pickar JH. Incidence of endometrial hyperplasia in postmenopausal women taking conjugated estrogens (Premarin) with medroxyprogesterone acetate or conjugated estrogens alone. The Menopause Study Group. Am J Obstet Gynecol. 1994;170(5 Pt 1):1213-23. doi: 10.1016/s0002-9378(94)70129-6
20. Ziel HK, Finkle WD. Increased risk of endometrial carcinoma among users of conjugated estrogens. N Engl J Med. 1975;293(23):1167-1170. doi:10.1056/NEJM197512042932303
21. Design of the Women's Health Initiative clinical trial and observational study. The Women's Health Initiative Study Group. Control Clin Trials. 1998;19(1):61-109. doi:10.1016/s0197-2456(97)00078-0
22.Rossouw JE, Anderson GL, Prentice RL, et al; Writing group for the Women's Health Initiative investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002;288(3):321-333. doi: 10.1001/jama.288.3.321
23. Anderson GL, Limacher M, Assaf AR, et al; Women's Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701-1712. doi: 10.1001/jama.291.14.1701
24. Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368. doi:10.1001/jama.2013.278040
25. Manson JE, Crandall CJ, Rossouw JE, et al. The Women’s Health Initiative randomized trials and clinical practice: A review. JAMA. 2024;331(20):1748–1760. doi:10.1001/jama.2024.6542
26. U.S. Food and Drug Administration. Menopause. December 14, 2023. Accessed April 10, 2025. https://www.fda.gov/consumers/womens-health-topics/menopause
27. The 2022 Hormone Therapy Position Statement of The North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. doi: 10.1097/GME.0000000000002028
28. US Preventive Services Task Force. Hormone therapy for the primary prevention of chronic conditions in postmenopausal persons: US Preventive Services Task Force Recommendation Statement. JAMA. 2022;328(17):1740–1746. doi:10.1001/jama.2022.18625
29. U.S. Food and Drug Administration. Menopause: Medicines to help you. August 22, 2019. Accessed April 10, 2025. https://www.fda.gov/consumers/free-publications-women/menopause-medicines-help-you
30. U.S. Department of Health and Human Services. Office on Women’s Health. Menopause Treatment. March 11, 2025. Accessed April 10, 2025. https://womenshealth.gov/menopause/menopause-treatment
31. U.S. Food and Drug Administration. FDA approves novel drug to treat moderate to severe hot flashes caused by menopause. May 12, 2023. Accessed April 10, 2025. https://www.fda.gov/news-events/press-announcements/fda-approves-novel-drug-treat-moderate-severe-hot-flashes-caused-menopause
32. U.S. Food and Drug Administration. FDA adds warning about rare occurrence of serious liver injury with the use of Veozah (fezolinetant) for hot flashes due to menopause. September 12, 2024. Accessed April 10, 2025. https://www.fda.gov/drugs/drug-safety-and-availability/fda-adds-warning-about-rare-occurrence-serious-liver-injury-use-veozah-fezolinetant-hot-flashes-due
33. National Institute of Health. National Library of Medicine. DAILYMED. Paroxetine capsule. September 1, 2023. Accessed April 10, 2025. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=1383d713-79b9-45bd-bd06-65707f28bc99
34. National Institute of Health. National library of medicine DAILYMED. Raloxifene hydrochloride tablet. September 24, 2014. Accessed April 10, 2025. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f4fe353-c5de-44ba-9c68-b75a185f7dc5
35. National Institute of Health. National library of medicine DAILYMED. Osphena. March 16, 2023. Accessed April 10, 2025. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8462d6ab-e3cd-4efa-a360-75bf8f917287
36. National Institute of Health. National library of medicine DAILYMED. DUAVEE- conjugated estrogens/bazedoxifene tablet, film coated. January 13, 2025. Accessed July 15, 2025. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e16705d8-4472-4f83-96ac-69fa2be066cb
37. “The 2023 Nonhormone Therapy Position Statement of The North American Menopause Society” Advisory Panel. The 2023 nonhormone therapy position statement of The North American Menopause Society. Menopause. 2023;30(6):573-590. doi:10.1097/GME.0000000000002200
38. Iyer TK, Fiffick AN, Batur P. Nonhormone therapies for vasomotor symptom management. Cleve Clin J Med. 2024;91(4):237-244. doi:10.3949/ccjm.91a.23067
39. Guttuso T Jr, Kurlan R, McDermott MP, Kieburtz K. Gabapentin's effects on hot flashes in postmenopausal women: a randomized controlled trial. Obstet Gynecol. 2003;101(2):337-45. doi: 10.1016/s0029-7844(02)02712-6
40. Butt DA, Lock M, Lewis JE, Ross S, Moineddin R. Gabapentin for the treatment of menopausal hot flashes: a randomized controlled trial. Menopause. 2008;15(2):310-8. doi: 10.1097/gme.0b013e3180dca175
41. National Institutes of Health. National Center for Complementary and Integrative Health. Menopausal symptoms: in-depth. May 2017. Accessed April 25, 2025. https://www.nccih.nih.gov/health/menopausal-symptoms-in-depth
42. U.S. Department of Health and Human Services. Office on women’s Health. Menopause and your health. March 12, 2025. Accessed April 10, 2025. https://womenshealth.gov/menopause/menopause-and-your-health
43. National Institutes of Health. National Institute on Aging. Infographic: Staying healthy during and after menopause. January 27, 2025. Accessed April 10, 2025. https://www.nia.nih.gov/health/menopause/staying-healthy-during-and-after-menopause
44. Centers for Disease Control and Prevention. Women’s Health. Age is just a number: health tips for women over 50. September 23, 2024. Accessed April 10, 2025. https://www.cdc.gov/womens-health/features/age-just-a-number.html