Learning Objectives
After completing this application-based continuing education activity, pharmacists will be able to
| Review basic intramuscular technique for vaccine administration |
| List changes in administration technique that increase safety and decrease patient pain |
| Describe the "clean as you go" process that saves time and reduces error |
After completing this application-based continuing education activity, pharmacy technicians will be able to:
| Review basic intramuscular technique for vaccine administration |
| List changes in administration technique that increase safety and decrease patient pain |
| Describe the "clean as you go" process that saves time and reduces error |

Release Date: January 9, 2024
Expiration Date: January 9, 2027
Course Fee
FREE
There is no funding for this CE.
ACPE UANs
Pharmacist: 0009-0000-24-005-H06-P
Pharmacy Technician: 0009-0000-24-005-H06-T
Session Codes
Pharmacist: 21YC03-ABC28
Pharmacy Technician: 21YC03-CBA24
Accreditation Hours
1.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-24-005-H06-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
Jill M. Fitzgerald, PharmD
Emeritus Associate Professor of Clinical Pharmacy
University of Connecticut School of Pharmacy
Storrs, CT
Jeannette Y. Wick, RPh, MBA
Director, Office of Pharmacy Professsional Development
University of Connecticut School of Pharmacy
Storrs, CT
Gabriella Scala
PharmD Candidate 2022
University of Connecticut School of Pharmacy
Storrs, CT
Samuel Breiner
PharmD Candidate 2021
University of Connecticut School of Pharmacy
Storrs, CT
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Jill Fitzgerald, Samuel Breiner, Gabriela Scala and Jeannette Wick have no relationships with ineligible companies.
ABSTRACT
Over the next months, we expect that more people will receive intramuscular vaccines than ever before. Many pharmacists and in some cases, pharmacy technicians, will mobilize to help with the immunization efforts. Some will take training for the first time, and others will have been trained but rusty. This activity reviews the best practices associated with intramuscular injection. UConn School of Pharmacy is providing this continuing education activity free as a public service.
CONTENT
Content
INTRODUCTION
As the healthcare community mobilizes and begins vaccinating to prevent the spread of coronavirus-SARS-19, pharmacists and in many places pharmacy technicians will be called to assist. In an effort to engage Americans in the program and encourage vaccination, the media is full of stories and videos of people receiving vaccinations. We at the University of Connecticut School of Pharmacy have watched with great interest, reading national newspapers and watching television clips about vaccination. One comment posted in response to an article in the New York Times caught our attention. Someone who dubbed herself “Retired Nurse” wrote the following comments1:
“As for sore arms, I am not surprised. The wide variation in injection techniques displayed on television have been horrendous: Slow, tentative needle insertions, not stabilizing the site, too high up in the shoulder, exceptionally large needle lengths in tiny arms, etc. make me cringe. Hilariously, they showed doctors ceremoniously giving some of them on television but let's be honest, most physicians do not routinely administer shots. That task is delegated to a nurse or even a medical assistant in doctors' offices in many states. A vaccination can be a lot less painful, if not virtually painless, with good injection training.”
We could not agree more, and as we prepare to train people from a number of professions in our state, we decided to create this short continuing education homestudy to help you review injection technique and stay abreast of the most recent developments.
Intramuscular Injections
Vaccines administered in pharmacies are generally given by one of two routes: (1) intramuscularly, or (2) subcutaneously. Most (but not all) immunizations are given intramuscularly. Most inactivated vaccines are administered intramuscularly in the deltoid, whereas all live-attenuated injectable vaccines are administered subcutaneously in the anterior arm (midway between the elbow and armpit).2 An exception of a common inactivated vaccine given subcutaneously would be meningococcal vaccine. To date, the available COVID-19 vaccines are all given intramuscularly. Intramuscular (IM) injections are exactly what the name implies – they are injections given into a muscle using a syringe.
Let’s review the parts of the syringe very quickly. A syringe has three primary parts. The needle, the barrel, and the plunger (see Figure 1). The needle is also called the “sharp,” and for vaccines, it’s a very fine needle. This is the distal part of the syringe that penetrates the skin. The barrel is the tube that holds the vaccine, and it has markings similar to that on a ruler. In most cases, the barrel measures milliliters (mL). The plunger is the plastic device used to pull the vaccine into and push the vaccine out of the syringe.
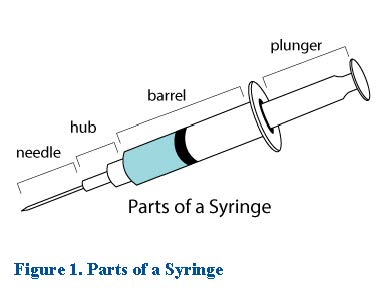
An important area of the syringe is called the hub or the hilt. This is the place where the needle meets the barrel. When penetrating the skin, you will push the needle all the way to the hub or the hilt. Before you inject, the entire needle will be in the skin and the muscle – you won’t be able to see any of the metal needle. Many people worry that they will hit the patient’s bone. It’s a comfort to know that if you hit the bone, you will feel it. The patient will not. This is a word-for-word explanation that our peer reviewer and authors like3:
"Needle length should be chosen based on the body habitus and weight of the patient. A needle that is too long can penetrate the deltoid muscle, hitting the bone. Although patients will not feel their bones being hit, the vaccine might not fully absorb into the muscle, leading to a reduced immune response. Furthermore, if the needle is too short the vaccine might be administered subcutaneously, which might result in decreased immune response and the development of nodules or cellulitus."
Good Technique
Good technique starts with preparation. Before you start administering vaccines, it’s essential that you prepare and anticipate how many patients you’ll see and what their needs will be. A cornerstone of good technique is knowing exactly how you will document. Especially with the COVID-19 vaccine, knowing how to document will be essential. Our understanding is that a new Vaccine Administration Management System has been developed to capture that data. When you arrive at your site, and eventually when the vaccine is available in your pharmacy, someone should train you on how to use the Vaccine Administration Management System. As with all vaccines, you’ll need to document the patient’s name, the vaccine’s lot number and expiration date, and where you gave the vaccine (left deltoid, right deltoid, etc.).4 And here is a quick aside: Many pharmacies don’t do a good job of documenting vaccines they give in their medication systems. Be certain to know what documentation is necessary, either in addition to or instead of Vaccine Administration Management System. For instance, health systems will require documentation in their electronic medical records or pharmacy system.
Before you start, survey your area and ensure that the station at which you vaccinate has a sufficient amount of supplies. Table 1 lists items that you need at your station at all times and items you have to have ready for each patient. One thing we wish to emphasize is a technique that one of our students taught us. When you have gloves on, it’s very difficult to open a Band-Aid and apply it. In anticipation of needing it, if you peel back the outer wrapper before you start, it will be much easier to use the Band-Aid should you need it after vaccination. Some people even place the small opened section of the bandage on the patient’s skin right next to where they will inject, so it’s easy access. And note that often, if you have good technique, the patient will not bleed. But use a Band-aid in case they “spring a leak” later.
Table 1. Necessary Supplies for Immunization4,5
| Always at Your Station | Have Ready for Each Patient |
| • A sharps container
• A handy trash can • Band-Aids • Cleaning solution • Your personal protective equipment (mask, face shield, gloves) • A box of tissues
|
• One alcohol wipe
• One sterile 2 x 2 gauze pad • A new needle and syringe that are the correct size • A clean pair of disposable gloves (for you to wear) for each patient • A Band-Aid, partially open
|
Next, commit to cleaning as you go. Have you ever noticed that when you go to any fast food restaurant, it is always clean and organized? That’s because they teach their staff to clean as they go. This lesson, when employed in our homes and in our workplaces, is extremely useful. It’s especially useful when you are immunizing many people. You don’t accumulate trash that has to be picked up later. This process has three key points when it comes to immunization4,5:
- Throw paper and miscellaneous trash away immediately. What this means is if you take the cap off the needle, throw it in the trash immediately. You won’t be using the cap because we don’t recap needles any longer. Throwing it in the trash ensures you won’t be tempted to recap the needle. Similarly, any paper trash generated from anything that you open should go into the trash can immediately.
- After you inject and withdraw the needle from the muscle, activate the safety device on the needle using a hands-free method immediately.
- Place used needles or sharps in the sharps container as soon as you finish with them. Do not place the used syringe on your work area even for a moment. Put it in the sharps container. (Yes, we are stressing this point!)
Have a Seat, Please
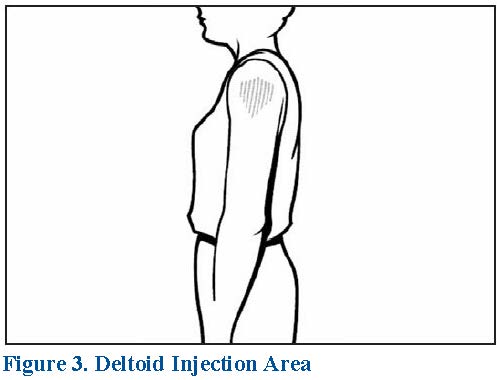
It’s critical for patients to be seated when you give injections. Ideally, you should be seated also and we will discuss why below. Ask patients to relax their arms. They can place their palms on their legs or dangle their arms at the sides. Completely expose the upper arm and find your upside-down triangle target area of the deltoid muscle. If administering more than one vaccine in the same arm, separate the injection sites by one inch so that any local reactions can be differentiated.6
As we implied above, for most adults, we administer the COVID-19 and most other IM vaccines in the upper arm. This is the location of the deltoid muscle. You will give the injection in the center of an upside-down triangle. To give the vaccine, completely expose the patient’s upper arm, and feel for the bone that goes across the top of the upper arm. This is the acromion process. The bottom of the acromion process is the flat edge of the inverted triangle (see Figures 2 and 3).5 The triangle points down. It ends at about the level of the armpit. You will inject into the lower two thirds of the deltoid. Note that giving injections in the upper third of the deltoid can damage the muscle and cause inordinate pain.7-9
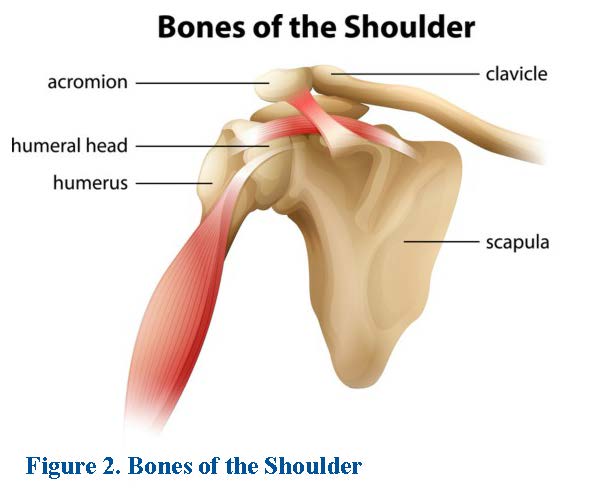
Shoulder injury related to vaccine administration (SIRVA) is an emerging concern. 3,7-9 This occurs when immunizers inject vaccines into the subdeltoid bursa or within the joint space. SIRVA causes shoulder pain and limited range of motion within 48 hours after IM vaccine administration.10,11 Experts advise immunizers to avoid administering vaccines in the top one-third of the deltoid. Studies show that immunizers who sit and administer vaccines to seated patients, using needles of the appropriate length, reduce the risk of SIRVA.7,8,12
Let’s get more specific. The correct area to give an injection is in the center of the triangle. You would inject one to two inches or two to three finger widths below the lower edge of the acromion process.5,14 Gently stretch the skin around the injection site with your non-dominant hand. This displaces the subcutaneous tissue, aids needle entry and reduces pain. Insert the needle at a 90 degree angle, all the way to the hub. Depress the plunger at a rate of 1 second for every 0.1 ml of fluid.13 Again, avoid injecting too close to the top of the arm. Don’t use this site if a person is very thin or the muscle is very small. In these cases, it’s better to inject into the anterolateral thigh.4 The SIDEBAR describes considerations when selecting needles size and length.
A final word before we go to the actual injection process. Please don’t say, “This will not hurt a bit!” People have very different thresholds for pain and it’s impossible to predict whether it will hurt. Develop some language that you are comfortable with, and use it. A good response of people who ask if it will hurt is to say, “It may hurt or sting a little but just for a minute or two.”
Prepare yourself before you give an injection by using personal protective equipment, and using it correctly.4 During the pandemic, we advise covering your nose and your eyes, keeping your hands away from your face, and washing your hands often. Practice good hygiene before and after immunizing each patient. Do not wear the same set of gloves for more than one patient. Change gloves between patients and wash your hands and sanitize (and let dry) before putting on a new pair of gloves.4,5
SIDEBAR: Choosing the Right Needle4,5,14-17
Immunizers will administer current COVID-19 vaccine from Pfizer and Moderna using needles that fall in the ranges of 22-25 gauge and 1-1.5 inches in length. Remember, the higher the gauge, the finer the needle! The Pfizer COVID vaccine is currently approved for ages 16 and older while the Moderna vaccination has approval for ages 18 and older. CDC vaccination recommendations on needle gauge and length are consistent with current Pfizer and Moderna recommendations. The table below summarizes CDC recommendations on general needle gauges and lengths for IM injections based on age.
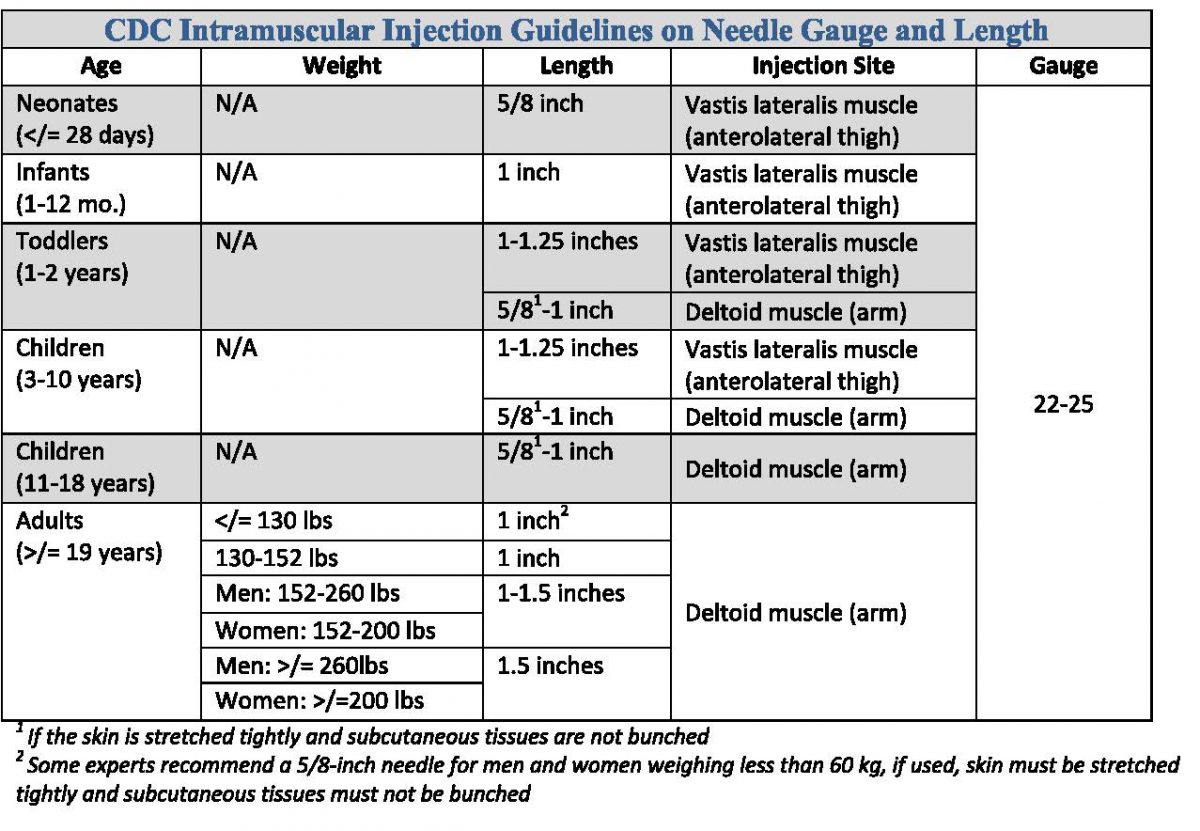
Although we may be injecting 1 to 1.5-inch needles into patients' deltoids now, our near future will consist of younger and frail patients. This may require use of shorter needles (i.e., 5/8 inch) and a different injection site - that being the vastus lateralis (a muscle on the outer thigh).
Ready, Set, Go
Let’s go through the process twice and review first the general procedure, then some specifics.
Here are the steps4,14:
- First, open the alcohol wipe. Wipe the area where you plan to give the injection.
- Prepare the needle.
- Hold (stretch) the skin around where you will give the injection.
- Insert the needle into the muscle at a 90° angle, all the way to the hub.
- Inject the vaccine at a rate of 0.1 ml per second.
- Remove the needle at the same 90 degree angle.
Now let’s review some nuances.4,5,14
- First, open the alcohol wipe. Wipe the area where you plan to give the injection. Wiping in a circular motion from the center out sometimes increases circulation and desensitizes the area. However, there’s no need to scrub. Just wipe firmly and dispose of the used alcohol wipe and its wrapper. Let the area dry (approximately 30 seconds) and do not blow on or touch the area until you give the injection.
- Prepare the needle. Hold the syringe with your dominant hand and pull the cover off with your other hand. Throw the cover in the trashcan immediately so you are not tempted to recap. Place the syringe between your thumb and first finger (like a dart). Let the barrel of the syringe rest on your finger.
- Hold the skin around where you will give the injection. With your free hand, which is also your non-dominant hand, gently press on the skin and pull it so that it’s slightly tight. Experts recommend two different ways of doing this. One is to make a “C” with your nondominant hand and stretch the skin between your first finger in your thumb. The second is to use the outer edge of you hand below the pinkie finger and pull the patient’s skin taut by pushing toward the outer edge of the arm (toward your non-dominant hand).
- Insert the needle into the muscle. Hold the syringe barrel tightly and inject the needle through the skin and into the muscle at a 90° angle.
- Inject the vaccine. Push down on the plunger and inject the medicine using your index finger. Push firmly and steadily at a rate of about 0.1 mL per second. Note that the Pfizer COVID-19 vaccine is only 0.3 mL, so you can inject it in about three seconds. The Moderna COVID-19 vaccine is a 0.5 mL volume, so it will take five seconds to inject.
- Remove the needle. Once you have injected the vaccine, remove the needle at exactly the same angle as you used for it to go in – that is, 90°. Activate the safety device and dispose of the entire syringe in your sharps container. You can place gauze over the area where you give the injection or cover the injection site with a Band-Aid (do not massage the area).
SIDEBAR: Needle Safety4,18
Now let's quickly discuss how we can keep ourselves safe while immunizing. The CDC estimates that 590,194 needlestick injuries occur annually in all healthcare settings. Immunizing exposes pharmacists to an increased risk of needlestick injury and transmission of bloodborne disease, with the most dangerous being hepatitis B, hepatitis C, and HIV. Therefore, if we are to know the perfect technique to immunize we must also know the perfect technique to keep ourselves safe.
Prevention is key to avoiding needlestick injury. Prevention includes:
- NEVER recapping needles by hand (if you absolutely must recap a syringe by hand, use a one-handed method and scoop the cap onto the needle. That is, place cap on a flat surface, remove your hand from the cap, insert the syringe needle tip deep into the cap, and press the tip of the cap against an inanimate object to secure it in place)
- Disposing of used needles in sharps containers
- Use needles with safety features, called "engineered injury protection"
- NEVER handing a syringe with an uncapped needle to someone else
If a needlestick injury should occur, you must be equipped with the knowledge of what to do next.
- Needlestick/cut: wash with soap and water
- Splashed on skin or in nose or mouth: flush with water (soap if possible)
- Splashed in eyes: irrigate with clean water, saline, or sterile irrigants
Be sure to report the incident to your supervisor and seek medical treatment to discuss possible risk of exposure or need for post-exposure treatment. Keeping ourselves safe is just as important as keeping our patients safe.
Refining Technique
So now we’ve reviewed the step-by-step process for giving an IM vaccine. Let’s talk about a few points that will refine your technique and make you a real pro.
As we prepare to vaccinate an entire nation, pharmacists will be working side-by-side with people from many different healthcare disciplines. In fact, we may be working with people who are not healthcare providers but have simply been trained to administer immunizations. From our experience, we have learned that conflict sometimes arises because healthcare practitioners trained in different disciplines have different ways of doing things. Our intent is to follow the most recent expert advice and use best practices. For that reason, we want to point out a few things that are either so new that others may not be aware of them or different from what you may see or hear at immunization sites.
First, some helpful observers may tell you that you need to aspirate before you inject. For many years, many healthcare professionals were trained to aspirate – meaning after the needle is in the muscle, the immunizer will pull back on the plunger and see if they draw up any blood. This is an outdated practice.14 The Centers for Disease Control and Prevention indicates that aspiration is unnecessary and unwarranted when administering vaccines. They indicate, “Aspiration before injection of vaccines or toxoids (i.e., pulling back on the syringe plunger after needle insertion but before injection) is not necessary because no large blood vessels are present at the recommended injection sites, and a process that includes aspiration might be more painful for infants.”4,19 Should another provider approach you and criticize your technique, telling you that you need to aspirate, feel free to educate them about the proper way to give a vaccine!
Second, while you are going through the immunization steps, you can help patients relax and build some confidence if you talk to the patient. A little chitchat will help patients feel comfortable. We probably don’t need to say this but we will: Stick with safe topics. Some good questions are things like, “Do you have a pet?” or “It’s really cold today, isn’t it?” Remember that it’s best to use open-ended questions once you get the conversation started, with open-ended questions being those that cannot be answered with a yes or a no. For example, if the patient responds affirmatively to your question about pets, keep the ball rolling by saying “What kind of pet do you have?” If you’re talking about the weather, you can ask the patient what his or her favorite season is, or what they like about rainy days. Asking, “What’s for dinner tonight?” is also of great conversation starter. It will also give you some ideas for your own supper!
Next, let’s talk about skin that is not clear or is discolored. Ideally, we would want to inject into an area of the skin that is clear. You should never inject into broken skin, moles, or rashy areas. While you can inject into tattooed skin, we advise against it. The reason for this is the same as the reason that we inject into the clear areas of the skin: we want to be able to see a local reaction if it develops.4
Finishing Up
Finally, we are ready to finish the process. Once you’ve administer the vaccine, you’ll need to direct patients about their next steps and what they need to do. With the current COVID-19 vaccines at the current time, patients need to stay at the immunization site for 15 minutes for observation or as directed by your site’s specific policy.20 This may change as we administer significantly larger numbers of vaccinations. Older pharmacists were trained to provide a vaccine fact sheet to every patient they immunize. That practice seems to be site-specific at this point, so if your site requires a vaccine fact sheet be given to patients, do that.
Review your documentation, and make sure that you have completed it entirely. This is critical for the COVID-19 vaccines because at some point, patients may need to prove that they were vaccinated to engage in certain activities. Take a few minutes to ensure that you have completed the documentation and submitted it appropriately.20
A last PRO TIP is to take a minute to look at your station. Ensure that you have enough supplies to continue immunizing patients. Do not overfill your sharps containers. Know where the “FULL” line is. When they are close to full ask for or retrieve an empty container as a backup. Sanitize the area as directed by your site in preparation for the next patient.
CONCLUSION
Even the most proficient immunizer sometimes faces dilemmas in the immunization clinic. A final PRO TIP is indispensable: If at any time you encounter a problem and you are unsure or uncomfortable, find a more experienced immunizer and ask for help. We see all kinds of issues when we immunize—people who experience vasovagal syndrome (faint at the sight or thought of needles), people who are very thin or obese, people who have latex allergies and need to know if the vial’s stopper contains latex (neither the Pfizer or Moderna vaccine vials do). Finding someone with more expertise or simply collaborating with others to plan an approach is smart. It important to do your best to ensure the patient receives the vaccine; if you turn a patient away, he or she may not return.
Pharmacist and Pharmacy Technician Post Test (for viewing only)
Post Test
Immunization: A Quick Refresher: Perfect Intramuscular Injection Technique
1. When injecting a vaccine into the deltoid muscle, which area should you be certain to AVOID?
A. The lower 1/3 of the upside-down triangle in which the acromion process is the top edge
B. The middle 1/3 of the upside-down triangle in which the acromion process is the top edge
C. The upper 1/3 of the upside-down triangle in which the acromion process is the top edge
2. You have completed the steps necessary to prepare for injecting a vaccine. You are almost ready to insert the needle into the patient’s arm. What is the LAST STEP before inserting the needle?
A. Pinch the skin on both sides so it makes a “mountain” and inject into the scrunched skin
B. Use your non-dominant hand to pull the skin in one direction away from the injection site
C. Tell the patient that it will not hurt and inject in whatever way is most comfortable for you
3. After injecting the vaccine, removing the needle, activating the safety mechanism, and discarding the syringe in the sharps container, what should you do to ensure the medication is absorbed?
A. Nothing. If you have used good injection technique, your job is done!
B. Massage the area for approximately one or two minutes.
C. Apply a hot compress and have the patient hold it there for 15 minutes.
4. How quickly do most guidelines recommend to inject vaccines?
A. 1 mL/second
B. 0.1 mL/second
C. 0.01 mL/second
5. Why does the Advisory Committee for Immunization Practices recommend AGAINST aspiration when injecting vaccines?
A. It increases risk of bleeding that will be difficult to stop
B. It causes vaccine to leak from the muscle and decreases effectiveness
C. No large blood vessels are present at the recommended injection sites
6. Which of the following are the MOST COMMON bloodborne pathogens?
A. Hepatitis B, hepatitis C, and HIV
B. Influenza, coronavirus, and HIV
C. Pneumonia, pinkeye, and staphylococcus
7. Which of the following statements is TRUE?
A. Always recap needles by hand
B. Dispose of used needles in trash receptacles
C. Use needles with safety features
8. If you absolutely must recap a syringe by hand, how many hands should you use?
A. One
B. Two
C. Three (get someone else to help)
9. You are prepared to inject a vaccine and have uncapped the needle, and thrown away the cap. Your team leader enters the room and says she needs you immediately to answer some questions about your last patient. She has brought another immunizer to take over your station for 15 minutes. Which of the following is the BEST way to proceed?
A. Hand the syringe with the uncapped needle to your replacement so he can finish this patient’s vaccination and leave with the team leader.
B. Fish around in the trash can, find the cap, and recap the needle, and give the now-capped needle to your replacement to finish with this patient.
C. Tell the team leader that you have discarded the cap, and suggest you finish with your current patient since it will only be a few seconds.
10. You inadvertently squirt something from a used syringe into your eye. What do you do?
A. Irrigate with clean water, saline, or sterile irrigants
B. Wash with soap and water
C. Flush with detergent and water
11. Which of the following would be considered an “engineered injury protection”?
A. Syringes with sliding sheath that shields the attached needle after use
B. Using an open container in which to dispose used needles
C. Asking employees for input on what needles they prefer
12. Select the statement that is TRUE for the current Pfizer and Moderna vaccines:
A. Both vaccines do not come with administration devices
B. Both must be stored in the refrigerator until 15 minutes before use
C. Both require needles that are 22-25 gauge and 1-1.5 inches in length
13. You greet a patient and ask him to uncover his deltoid. As you assess him, you notice that he must weigh at least 350 pounds. Which factor needs to be adjusted before you administer the vaccine?
A. The dose
B. The needle gauge
C. The needle length
14. Your patient looks at the syringe, pales, and begins to shake. She tells you that she has a “vasovagal” reaction to needles. You do not know what this means. What is the BEST way to proceed?
A. Distract her with idle chit-chat
B. Find a more experienced immunizer
C. Tell her she will have reschedule
15. Patients can be quirky. Your current patient wants to stand to receive the vaccination. What is the BEST explanation for why both of you should sit?
A. Immunizers who sit and administer vaccines to seated patients reduce the risk of injury to the patient’s shoulder.
B. Immunizers who sit and administer vaccines to seated patients reduce the risk of needlestick injury to the immunizer.
C. Immunizers who stand and administer vaccines to seated patients reduce the risk of the patient fainting.
16. Your patient is heavily tattooed. In this training, we emphasized the importance of finding the area of clearest skin. Why?
A. We want to be able to see a local reaction if it develops.
B. Injecting into tattooed skin is more painful for the patient.
C. Current COVID vaccines cannot be given in a tattooed area.
17. What is the proper angle to give an IM injection?
A. 45o
B. 90o
C. Inject at 45o, withdraw at 90o.
18. Which of the following questions should you be prepared to answer in case a patient asks?
A. Does the vaccine’s vial have plastic in the stopper?
B. Does the vaccine’s vial have latex in the stopper?
C. Does the vaccine come in a multidose vial?
19. What is the BEST position for a patient’s arm while you are giving an IM injection?
A. Relaxed with palms on legs or arm dangling at sides
B. Taut with the patient squeezing a rubber ball
C. Flexed as if they were showing you the size of their deltoid
20. You’ve vaccinated a patient with a COVID vaccine, disposed of the sharp, and finished your task. What is the BEST thing to tell the patient?
A. Thanks for doing this, your nation appreciates you.
B. See you for the follow-up dose in six weeks!
C. Please remain in the clinic for 15 minutes.
References
Full List of References
References
1. Harmon A. What the Vaccine Side Effects Feel Like, According to Those Who’ve Gotten It. Available at https://www.nytimes.com/2020/12/28/us/vaccine-first-patients-covid.html. Accessed December 30, 2020.
2. Wick JY. Immunization: Tips, tools, and total success. Available at https://www.pharmacytimes.com/publications/issue/2016/August2016/Immunization-Tips-Tools-and-Total-Succes. Accessed January 2, 2020.
3. Bancsi A, Houle SKD, Grindrod KA. Getting it in the right spot: Shoulder injury related to vaccine administration (SIRVA) and other injection site events. Can Pharm J (Ott). 2018;151(5):295-299.
4. Centers for Disease Control and Prevention. Vaccine administration. Available at https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/administration.html. Accessed December 30, 2020.
5. Centers for Disease Control and Prevention. Vaccine Administration: Intramuscular (IM) Injection Children 7 through 18 years of age. Available at https://www.cdc.gov/vaccines/hcp/admin/downloads/IM-Injection-children.pdf. Accessed December 30, 2020.
6. Centers for Disease Control and Prevention. Adminster the vaccines. Available at https://www.cdc.gov/vaccines/hcp/admin/administer-vaccines.html. Accessed January 3, 2021.
7. Bodor M, Montalvo E. Vaccination-related shoulder dysfunction. Vaccine. 2007;25(4):585-587.
8. Atanasoff S, Ryan T. Lightfoot R, Johann-Liang R. Shoulder injury related to vaccine administration (SIRVA). Vaccine. 2010;28(51):8049-8052. doi: 10.1016/j.vaccine.2010.10.005.
9. Cook IF. Subdeltoid/subacromial bursitis associated with influenza vaccination. Hum Vaccin Immunother. 2014;10(3):605-606. doi:10.4161/hv.27232.
10, National Vaccine Injury Compensation Program (VICP). Prevention of SIRVA. Health Resources and Services Administration website. Available at hrsa.gov/advisorycommittees/childhoodvaccines/meetings/20150604/sirva.pdf. Accessed December 30, 2020.
11. Cross GB, Moghaddas J, Buttery J, Ayoub S, Korman TM. Don’t aim too high: avoiding shoulder injury related to vaccine administration. Aust Fam Physician. 2016;45(5):303-306.
12. Kroger AT, Sumaya CV, Pickering LK, Atkinson WL. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60(RR02):1-60.
13. : Dougherty L, Lister S (2015) The Royal Marsden Hospital Manual of Clinical Nursing Procedures. Oxford: Wiley-Blackwell.
14. Immunize.org. How to administer intramuscular and subcutaneous vaccine injections. Avaialble at https://www.immunize.org/catg.d/p2020.pdf. Accessed January 3, 2021.
15. Centers for Disease Control and Prevention. Moderna COVID-19 vaccine. Available at https://www.cdc.gov/vaccines/covid-19/info-by-product/moderna/downloads/standing-orders.pdf. Accessed January 3, 2021.
16. Centers for Disease Control and Prevention. Pfizer-BioNTech COVID-19 Vaccine. Available at https://www.cdc.gov/vaccines/covid-19/info-by-product/pfizer/downloads/prep-and-admin-summary.pdf. Accessed January 3, 2021.
17. Centers for Disease Control and Prevention. Vaccine administration: Needle gauge and length. Available at https://www.cdc.gov/vaccines/hcp/admin/downloads/vaccine-administration-needle-length.pdf. Accessed January 3, 2021.
18. U.S. Government Printing Office. Needlestick Safety and Prevention Act. Available at http://www.gpo.gov/fdsys/pkg/PLAW-106publ430/html/PLAW-106publ430.htm. Accessed January 3, 2021.
19. Ipp M, Taddio A, Sam J, Gladbach M, Parkin PC. Vaccine-related pain: randomised controlled trial of two injection techniques. Arch Dis Child. 2007;92(12):1105-1108. DOI: 10.1136/adc.2007.118695
20. Centers for Disease Control and Prevention. Resource library. Available at https://www.cdc.gov/vaccines/hcp/admin/resource-library.html. Accessed January 3, 2021.