Learning Objectives
After completing this knowledge-based continuing education activity, pharmacists will be able to
| · Discuss the prevalence and consequences of SUDs |
| · Describe the components of SBIRT |
| · Recognize motivational interviewing skills to promote readiness to change |
| · Discuss harm reduction and how it pertains to SUDs |
| · Describe barriers associated with the use of SBIRT in the community setting |
After completing this knowledge-based continuing education activity, pharmacy technicians will be able to
| · Discuss the prevalence and consequences of SUDs |
| · Describe the components of SBIRT |
| · Discuss harm reduction and how it pertains to SUDs |
| · Describe barriers associated with the use of SBIRT in the community setting |

Release Date:
Release Date: September 7, 2022
Expiration Date: September 7, 2025
Course Fee
Pharmacists: $7
Pharmacy Technicians: $4
There is no grant funding for this CE activity
ACPE UANs
Pharmacist: 0009-0000-22-051-H08-P
Pharmacy Technician: 0009-0000-22-051-H08-T
Session Codes
Pharmacist: 22YC51-YXT24
Pharmacy Technician: 22YC51-TXY69
Accreditation Hours
2.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-22-051-H08-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
Helen Pervanas, PharmD
Professor of Pharmacy Practice
Massachusetts College of Pharmacy and Health Sciences School of Pharmacy
Worcester/Manchester, MA
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Dr. Pervanas has no relationship with ineligible companies and therefore has nothing to disclose.
ABSTRACT
Hazardous use of alcohol and or opioids can result in harm. If not treated, this hazardous use could develop into a Substance Use Disorder (SUD). SUDs are associated with poor health related outcomes and increased healthcare costs. Screening, brief intervention and referral to treatment (SBIRT), is a public health approach to identify persons with at-risk behaviors and minimize the development of SUDs. The premise behind SBIRT is to promote early intervention with at-risk users and minimize harm. The screening process determines the severity and risk level of a person’s substance use and risk of misuse. Based on the results, healthcare professionals can perform a brief intervention and or a referral to treatment. Healthcare professionals such as pharmacists and pharmacy technicians can use SBIRT to identify and intervene on behalf of persons that are at risk of an SUD. Healthcare providers can perform SBIRT in many healthcare settings including community pharmacies, hospitals, and primary care offices.
CONTENT
Content
Introduction
Substance Use Disorders (SUDs), continue to be a major concern in the United States. In 2017, nearly 20 million people reported an SUD because of alcohol or illicit drug use.1 Costs associated with substance abuse are approximately $249 billion dollars for alcohol and $193 billion dollars for illicit drugs.2-4
Alcohol use is second to nicotine for substance use among all substances misused.1 In 2017, 140 million persons aged 12 and older reported alcohol use. A total of 16.7 million reported heavy alcohol use of five or more days over a 30-day timespan. Heavy alcohol use is defined as drinking four or more drinks on one occasion for females and five or more drinks in males. Heavy alcohol use can result in several health-related concerns, to include cirrhosis, depression, cancer, neuropathy, and pancreatitis to name a few.5
Typically, clinicians often treat people who have SUDs after they have developed the condition.6,7 Other approaches include inpatient or outpatient treatment programs for those with SUDs and prevention programs to educate and inform the public of the dangers associated with substance use.
An alternative approach to these methods is to identify persons with at-risk behaviors for substance misuse and provide interventions to reduce long-term use and harm. This approach is called SBIRT. SBIRT stands for Screening, Brief Intervention, and Referral to Treatment.7 This evidence-based approach addresses harmful behaviors BEFORE they escalate to a full-blown SUD.
Who can perform SBIRT?
Many healthcare professionals can perform SBIRT, including doctors, nurses, pharmacists, pharmacy technicians, and behavioral health specialists. SBIRT is also adaptable to a team-based approach. Pharmacists and pharmacy technicians are in a particularly good position to perform SBIRT, as they are accessible, especially in community pharmacy settings.8 SBIRT can also be applied in several clinical settings, such as hospitals and ambulatory care clinics.
SBIRT’s first step involves the screening process. Using a universal screening approach is an important point of the screening process. A universal approach means screening everyone, regardless of who they are, or how they look or act. This makes sense because clinicians cannot determine if someone is using alcohol or other substances based on appearance and behavior. Pharmacists and pharmacy technicians can screen patients in any pharmacy setting to include community, hospital, and ambulatory care. In busy community settings, a targeted approach may be necessary. With targeted approaches, pharmacy teams might screen individuals who are on opioids, benzodiazepines, and other medications that have the potential for abuse. Ideally, however, the universal approach is better. If we focus only on certain populations, we may target individuals who don’t have an SUD and overlook someone who has an SUD but takes no prescription medications. The initial screening question is simple: a single yes/no question that determines if further screening is necessary.
PAUSE AND PONDER: When and where would you use SBIRT in your pharmacy practice?
How to Perform SBIRT in a Community Pharmacy Setting
Many pharmacy team members think that they cannot or should not perform SBIRT in their settings. With pharmacy teams expanding their responsibilities, it’s entirely possible to add SBIRT to the community pharmacy tool kit.
Community pharmacy teams need to note that they do not need to perform SBIRT in its entirety. In some cases, pharmacists and technicians may only perform the screening and then refer the patient to a provider for treatment. Pharmacists can perform a brief intervention if opioid misuse is a concern. For example, the pharmacist may access the prescription drug-monitoring program and recognize the patient is seeing multiple providers and using several pharmacies to fill opioid prescriptions. In this case, the pharmacist can perform a screening and brief intervention with the patient to discuss safe opioid use and possible referral to treatment.
Roberta is a 27-year-old female who presents to the pharmacy with a prescription for oxycodone. The pharmacy technician enters the prescription information and notices that Roberta picked up a 30-day supply two weeks ago. The technician informs the pharmacist about the early refill. The pharmacist refers to the prescription drug-monitoring program and notices that Roberta filled two other opioid prescriptions from different doctors at two different pharmacies. The pharmacist screens Roberta and provides a brief intervention.
Pharmacists can refer a patient to treatment or provide information on treatment centers based on the discussion. For example, while engaging with the patient the pharmacist may recognize that the patient is purchasing needles/syringes for illicit drug use. This is a perfect opportunity for the pharmacist to provide a referral to treatment.
When screening for alcohol and drugs, healthcare providers use pre-screening questions developed by the National Institute of Alcohol Abuse and Alcoholism for alcohol and the National Institute of Drug Abuse for drugs. Pre-screening questions determine whether additional screenings are necessary.
For alcohol the pre-screening question is, “Do you sometimes drink beer, wine, or other alcoholic beverages?” If the individual answers no, no further screening is necessary. If the individual answers in the affirmative or screens positive for alcohol, the screener would perform additional screening based on the Alcohol Use Disorders Identification Test (AUDIT) to evaluate alcohol use further.9
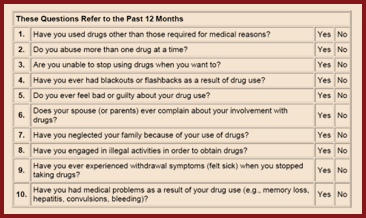
The same holds true for pre-screening for drug use. If an individual answers in the affirmative to the pre-screening question, “How many times in the past year have you used an illegal drug or a prescription medication for nonmedical reasons?” then the screener would use the Drug Abuse Screening Test (DAST-10) questionnaire to evaluate drug use further.10 (See Figure 1)
Figure 1. DAST-10 Questionnaire10
Let’s start with the AUDIT questionnaire. This 10-question screening tool addresses recent alcohol use, dependence symptoms, and harmful behaviors. (See Figure 2) Once the screening is complete, the scoring will determine next steps.
Figure 2. AUDIT Questionnaire9
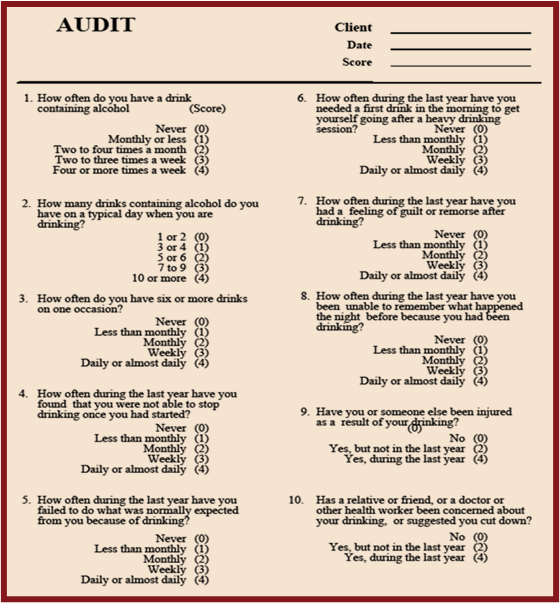
Some key points to consider when using the AUDIT are the recommended drinking limits and size of the beverage. Did you know that the serving size of a glass of wine is five ounces, and that one bottle of wine typically contains five glasses? A serving of beer is 12 ounces, and a serving of spirits (hard liquor) is one and one-half ounces. The screener should explain serving sizes to the patient to ensure an accurate account of alcohol consumption and score of the AUDIT.
Recommended drinking limits for men are two drinks/day and no more than 14 drinks/week and for women one drink/day and no more than seven drinks/week. For those 65 or older, the recommended limits are similar to women: one drink/day and no more than seven drinks/week.11 Consuming more than the recommended limits can result in binge drinking which is associated with greater harm and dependence. Binge drinking is five or more drinks for men or four or more drinks for women, and people who are 65 or older.12
The AUDIT score determines the severity and next steps that may include a brief intervention or referral to treatment. Individuals scoring between 0 and 7 are low risk and individuals scoring 20 or greater are considered dependent use and would benefit from a referral to treatment.
Pharmacy teams who are familiar with other screening methods may recall that a positive binge drinking finding would require an intervention using those methods. Using the AUDIT, binge drinking alone may not require an intervention. The intervention or referral to treatment would depend on the overall score of the AUDIT.
Scoring the AUDIT
Dependent Use (20+)
Harmful Use (16‒19)
At-Risk Use (8‒15)
Low Risk (0‒7)
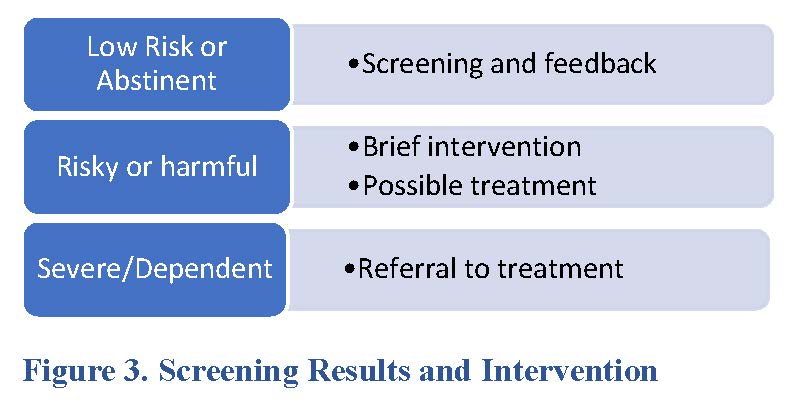
The screening process for drugs is like that used for alcohol. The DAST-10 questionnaire assesses drug use in the past 12 months. (See Figure 1) Interpretation of the results determines the suggested action. Figure 3 describes screening results and suggested intervention. For example, a score of between 3 and 5 using the DAST-10 suggests harmful use and moderate degree of problems related to drug use.
Scoring the DAST-10
High Risk (6+)
Harmful Use (3‒5)
Hazardous Use (1‒2)
Abstainers (0)
Once the screener completes the screening, the score determines next steps for the patient. Next steps could include feedback, brief intervention, and or a referral to treatment. (See Figure 3.) For example, in persons with a low risk, feedback can include discussing the results of screening and risk of harm. A brief intervention is recommended in persons with risky or harmful behavior based on screening results.
Perform a screening for alcohol and drug use using a patient case
Joe is a 32-year-old man who hurt his back three years ago in a car accident. He has used opioids since the accident, but he still complains of pain. He supplements his medications by purchasing additional opioids online and on the street. Joe also has a history of alcohol use. He consumes three to four beers on most days. His family is concerned with his alcohol and drug use and recommends he seek help.
Below are his responses to the AUDIT and DAST-10 questionnaires. Based on his responses to the questions calculate his risk level for alcohol and drug use. See Tables 1 and 2.
Table 1. AUDIT Screening for Joe
| Question | Answer | Score |
| How often do you have a drink containing alcohol? | Daily | 4 |
| How many drinks containing alcohol do you have on a typical day when you are drinking? | 4 | 1 |
| How often do you have six or more drinks on one occasion? | Once in awhile | 1 |
| How often during the last year have you found that you were not able to stop drinking once you had started? | Never | 0 |
| How often during the last year have you failed to do what was normally expected of you because of drinking? | Monthly | 2 |
| How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session? | Never | 0 |
| How often during the last year have you had a feeling of guilt or remorse after drinking? | Never | 0 |
| How often during the last year have you been unable to remember what happened the night before because of your drinking? | Never | 0 |
| Have you or someone else been injured because of your drinking? | No | 0 |
| Has a relative, friend, doctor, or other health care worker been concerned about your drinking or suggested you cut down? | Yes | 4
|
| Total Score | 12 |
Based on Joe’s responses to the AUDIT what is his score and risk level?
Based on his responses to the questions Joe scored 12 on the AUDIT, which puts him as at-risk-use.
Table 2. DAST-10 Screening for Joe
| Question | Answer | Score |
| Have you used drugs other than those required for medical reasons? | Yes | 1 |
| Do you abuse more than one drug at a time? | No | 0 |
| Are you unable to stop using drugs when you want to? | Yes– The pain gets too great | 1 |
| Have you ever had blackouts or flashbacks as a result of drug use? | No | 0 |
| Do you ever feel bad or guilty about your drug use? | No | 0 |
| Does your spouse (or parents) ever complain about your involvement with drugs? | Yes | 1 |
| Have you neglected your family because of your use of drugs? | No | 0 |
| Have you engaged in illegal activities in order to obtain drugs? | Yes | 1 |
| Have you ever experienced withdrawal symptoms (felt sick) when you stopped taking drugs? | Yes | 1 |
| Have you had medical problems as a result of your drug use (e.g., memory loss, hepatitis, convulsions, bleeding)? | No | 0 |
| Total Score | 5 |
Based on Joe’s responses to the DAST-10 what is his score and risk level?
Based on his responses to the questions Joe scored a five, which indicates harmful use. We will come back to Joe and determine next steps for him.
Summary of screening
- Screening is an important first step to determine the severity and risk level of substance use
- Use a universal screening approach
- Determine the level of risk and intervention based on screening results
- Pharmacists and pharmacy technicians can successfully perform screenings
Brief Intervention (BI)
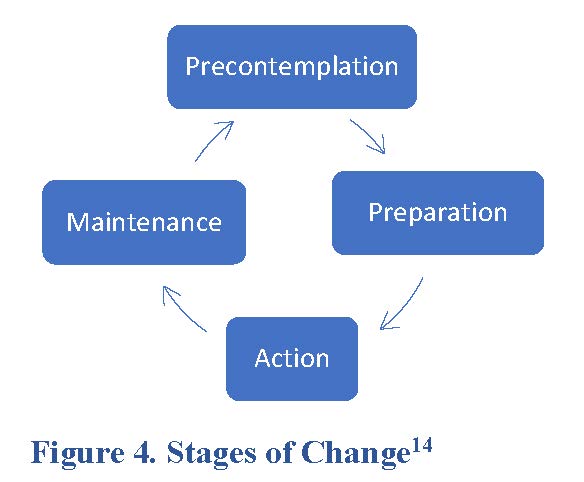
Following the screening process and based on the results, a BI may be necessary. A brief intervention, also referred to as a brief negotiated interview (BNI), can be performed by a healthcare professional such as a pharmacist, doctor, nurse, or behavioral specialist. Addiction experts recommend using a BNI for those with “at risk” or harmful level of risk based on screening results. During the BNI, the healthcare professional uses motivational interviewing (MI) to have a conversation with the patient and evoke the patient’s personal motivation for change.13 Before we talk more about BNIs, let’s talk about the five stages of change.14 Change happens gradually, and individuals can move through the different stages depending on the situation and can move in and out of the different stages. In pre-contemplation, individuals may not be ready to make a change. Figure 4 depicts the five stages of change.
Figure 4. Stages of Change14
MI has several components, which can be overwhelming and confusing. Here is a brief outline of the components.
Components of MI
- Key qualities of MI
- Basic Principles of MI
- BNI Process
- OARS Framework
What is a brief intervention’s purpose and how do we use MI to evoke change? Motivational interviewing is an evidence-based approach to changing behaviors.13,15
Key qualities of MI include13
- Facilitate communication between the healthcare professional and patient, where information and guidance is given
- Empower individuals to change based on what’s important to them
- Respect patient’s autonomy to facilitate change
Healthcare professionals can use MI to engage the patient as an equal partner. Although the name motivational interviewing suggests the healthcare professional is motivating the patient, that isn’t the case. MI is not a way to change individuals, make demands of patient, or instruct them what to do or not do. MI is a way to help examine situations and options for patients. MI is not easy to learn and takes practice. Pharmacists may find MI difficult to apply because counseling and instructing patients is part of everyday practice. MI is different and recognizes that patients are responsible for their actions and taking action to make changes.
MI can be very useful when people
- Have mixed feelings or are ambivalent about change
- Have low confidence about making changes
- May be uncertain about whether they want to make changes, creating low desire
- Are not clear about the benefits of change and concerns related to the current situation, so do not deem change important
MI is based on four basic principles15,16:
- Express empathy
- Develop discrepancy
- Roll with resistance
- Support self-efficacy
Expressing empathy is an important first step of the MI process. You do this by seeking to understand how the person feels without judgement. (See Side Bar-tips to express empathy)
Side Bar: Tips to Express Empathy
- Maintain eye contact but avoid staring
- Use reflective listening to hear and understand and repeat back the information
- Avoid sympathy, “I’m sorry this happened to you”
- Ask clarifying questions
- Avoid passing judgement
Developing discrepancy
Using this principle, the provider discusses the discrepancy between the patient’s values and behavior. This involves discussing the good and the bad related to the behavior. Most patients are aware of the dangers related to substance misuse but are ambivalent about making a change. Discrepancy between the patient’s goals and current behavior motivates change.
Roll with resistance
During the BNI, patients may become defensive when talking about their substance use. This resistance is often because of a fear to change. To decrease resistance, the healthcare professional can redirect the discussion for the patient to understand the harm associated with the behavior. Last, the provider can explore the pros and cons of the patient’s behaviors. For example, a patient may enjoy the euphoria of heroin use (pro) but conversely contracts a cellulitis infection (con).
Support self-efficacy
This guiding principle focuses on supporting patient goals. Patients may feel that they cannot meet goals or expectations. It is important that the provider believe in the patient and promote confidence to support change.
Here is an example of a brief intervention.
Cynthia is at the pharmacy having a discussion with the pharmacist. She is concerned about her alcohol use. The pharmacy technician performs the AUDIT screening and provides the results to the pharmacist for discussion. AUDIT Score: 15 “At-risk use”
Cynthia: “I have been drinking more often over the last few months.”
Pharmacist: “Tell me more about that, Cynthia.” (Reflective listening)
Cynthia: “Work has been very stressful, and alcohol helps me relax. I used to drink only socially on the weekends with friends but now I drink almost every day. My teenage daughter sees me drink every night and she tells me I should stop because it’s not good for me. I don’t want to be a bad role model for her.”
Pharmacist: “So you are saying that you drink alcohol almost every day so that you can cope with the stress at work?” (Reflective listening)
Cynthia: “Yes. I am using alcohol to cope with stress at work.”
As you can see by the conversation above, the pharmacist reflects on Cynthia’s concerns regarding stress and work, which cause her to drink alcohol to cope. The pharmacist makes no judgement on whether the behavior is bad or that she should stop drinking. The pharmacist applies reflective listening and expresses empathy.
Developing discrepancy looks at current behaviors versus future goals. Let’s continue the conversation with Cynthia and apply this principle.
Pharmacist: “It sounds like you are having a hard time at work. But you also love your daughter and want to be a good role model for her. Is that right?” (Developing discrepancy)
Here the pharmacist emphasizes Cynthia’s concerns with her alcohol use and how that affects her daughter. This is the discrepancy. This allows Cynthia to recognize the pros and cons of her alcohol use so that she may change her behavior.
In roll with resistance, patients may pushback stating that they don’t have a problem, or their drinking or drug use is not a problem. In this case, it may require further discussion of current behavior and negative effects related to that behavior. The correlation of cause and effect can motivate the patient to change.
Last, support self-efficacy, where patients are responsible for deciding on actions they will make to support change. This is important because patients take the responsibility of making changes.
Regardless of the stage, MI encourages the patient to express the desire to change or what is referred to as “change talk.” In change talk, look at the following: desire, ability, reasons and need or acronym DARN. See the example below based on the conversation with Cynthia earlier.
Desire: “I need to drink less alcohol.”
Ability: “I could find healthier ways of coping with the stress at work, like yoga or meditation.”
Reasons: “I want my daughter to be proud of me.”
Need: “I might lose my daughter.”
This “change talk” can prepare the individual to make changes and act on those changes. As mentioned earlier, MI is a collaborative approach between the patient and healthcare professional providing the brief negotiated interview and involves four fundamental processes. Let’s talk about each of the processes.
- Engage
- Focus
- Evoke
- Plan
Engage
Having an honest and open conversation that engages the patient is the first step in the process. Listening without passing judgement or trying to fix the problem is important. The OARS framework includes interactive techniques to engage the patient. OARS stands for open questions, affirmations, reflections, and summaries. Table 3 describes each element of the framework and purpose.
Table 3. OARS framework15
| Interview Skill | Description | Purpose |
| Open-ended questions | Ask the patient open-ended question vs. yes or no
|
Builds trust
Gathers information |
| Affirmations | Show empathy for the patient
Acknowledge the patient’s ability to make a change in their life Emphasize key points that are important to the patient.
|
Discuss/encourage patient’s abilities and healthy behaviors
Build the patient’s confidence and self-efficacy |
| Reflections | Listen and understand what the patient is saying and repeating back to the patient | Repeat back what was said
Incorporate unspoken feelings thoughts or behaviors |
| Summaries | Review key points of the conversation
Use reflective listening |
Help the patient see the big picture
Create an action plan Emphasize key points of the conversation |
Focus
During the conversation, focus on guiding patients to identify behaviors they struggle with or ambivalent to make a change. During the conversation, understand the patient’s dilemma or ambivalence. Asking what is important to them can help to identify the target and behavior that may inhibit them from reaching their goals.
Evoke
During the evoke process, we want patients to discuss their reasons for change and incorporate “change talk” during the conversation. Let’s go back to the conversation with Cynthia. Cynthia recognizes that she drinks alcohol to cope with the stress at work. She is also concerned that her drinking upsets her daughter and Cynthia wants to be a good role model. Her reason for change is that she wants to be a good role model for her daughter. Changing her behavior for her daughter is important to her.
Plan
The patient would commit to a plan of action that is simple, realistic, specific, and attainable. The patient should also set a timeline for the plan.
The incorporation of core skills is fundamental to MI. The acronym OARS, involves four interviewing skills to enhance motivation for change.15
Asking open-ended questions allows patients to provide more information and can provide insight to their feelings and thoughts. Close-ended questions only elicit a yes or no response with no further details. Here is an example of an open-ended versus close-ended question.
- Close-ended question: Do you drink alcohol often?
- Open-ended question: How much alcohol do you drink per week?
Affirmations
Statements of affirmation acknowledge the patient’s ability to make a change. Statements by the provider emphasize key points most important to the patient and support the patient to make changes.
Reflections
Reflections involve listening and understanding what the patient is saying. This can be as simple as repeating back the patient’s statements and incorporating the patient’s unspoken feelings or intent. Furthermore, reflections confirm with the patient that what you are repeating back is accurate. An example might be saying, “I heard you say that you have tried to stop drinking in the past and you have not been able to do it and I sense you are frustrated. Is that correct?” The latter statement incorporates the patient’s unspoken feelings and confirms an accurate account of the reflection.
PAUSE AND PONDER: Along the substance use continuum, with whom would you negotiate a reduction in use to lower risk levels?
Performing a BNI
A BNI uses MI to raise awareness in patients with risky or harmful substance use. Here are four important steps to follow when conducting a BNI.
Build rapport-raise the subject
Open the conversation by beginning with a general conversation and ask permission to discuss the topic of substance use. For example, you could say: “Thank you for meeting with me today. Would you mind speaking with me? Could I ask you some questions about your substance use?”
This engages the patient in the conversation. The conversation could highlight the patient’s substance use and explore the pros and cons of the situation. For example, with Cynthia, her alcohol use allows her to cope with stress at work. Conversely, her alcohol use makes her daughter upset and she wants to be a good role model for her. During the BNI, the provider should use open-ended questions to allow the patient to provide more information and further explore the patient’s substance use. Incorporating reflective listening, summarizing what the patient says, and weighing the pros and cons allows for decisional balance.
Provide feedback
After listening to the patient ask permission again to offer feedback based on the conversation. Review the screening results with the patient and connect consequences to substance use. Here is an example.
Karla is a 32-year-old mother of three children. She and her children are in the emergency department because of a car accident. Karla’s alcohol level is 0.09. (Blood alcohol levels ≥ 0.08% = legally impaired)
You perform a screening on Karla using the AUDIT. Her score reveals harmful use and when asked about her alcohol use causing injury, she states in the affirmative that she was under the influence of alcohol while driving with her children and feels extremely guilty and upset. During the conversation you ask permission to speak to Karla about her alcohol use and how this may be a direct cause of the accident. Karla may recognize the impact of her alcohol use and change her behavior.
Build readiness to change
Here we ask if they may be willing to make some changes. When doing so we can ask how willing they are or how ready they are to make a change. The provider can use a visual tool to assess willingness to change. This visual tool is a readiness ruler. (See Figure 5.) When approaching the patient, clinicians can use the readiness ruler in a way similar to that of a pain scale. For example, “On scale of 1 to 10, where 1 means you are not at all ready to change to 10 meaning you are very or completely ready to change. How ready are you to make a change about your substance use?”
Figure 5. Readiness Ruler15

PAUSE AND PONDER: What would be your response to a patient that states they are a 3 on the readiness ruler?
Negotiate a plan for change
Based on the screening results, the plan can vary. It may involve reducing risky use of substances and or a referral to treatment. The plan should be simple, realistic, specific, and attainable. Following up with patients to discuss changes and reinforcing the plan for change will promote long-term success.
Referral to Treatment
Patients diagnosed with an SUD by a provider or who have behaviors that are substance dependent (e.g., substance related injuries or inability to stop) or high-risk, such as increased frequency of substance use, require treatment. Healthcare professionals can easily refer the patient to treatment. Initiating the referral process by calling a trained treatment specialist on behalf of the patient to schedule an appointment can better assist the patient. Many resources are available to find treatment centers for patients. SAMHSA’s National Treatment Facility Locator is a helpful resource to locate a treatment center:17 http://findtreatment.samhsa.gov. Treatment options include counseling, medication assisted treatment, complimentary wellness, and support groups. The level of care is individualized and based on the severity of the substance use and comorbidities.
Key points for referral to treatment
- Make a plan with the patient
- Use a warm handoff
- Decide how you will communicate with the provider
- Confirm the plan with the patient
A warm handoff involves personally introducing the patient to the treatment provider. This helps build rapport and trust and increases the patient’s willingness to schedule an appointment. Warm handoffs are also more successful than passive referrals.
SBIRT in Practice
Healthcare professionals can utilize SBIRT in many areas of practice. Pharmacists and pharmacy technicians are one of the most accessible healthcare professionals, especially in community pharmacy settings. In this setting, pharmacists and pharmacy technicians can meet with patients to perform screenings, conduct a BNI, or refer to treatment, with the ultimate goal of reducing the risk of an SUD and patient harm.
Harm reduction is key to help to minimize adverse effects related to substance use.18 Harm reduction involves policies, programs, and practices that focus on the individual’s human rights. The goal of harm reduction is to keep people safe. Providers can reinforce positive changes in patients using MI. Examples of harm reduction include drug take back programs, access to naloxone, and syringe distribution.18 Distributing clean needles/syringes not only reduces harm for the persons using them but also contributes to community safety by reducing the spread of HIV, hepatitis, and other blood borne diseases.
Sadly, in community pharmacy settings, several barriers exist. Some include lack of privacy, lack of staffing, lack of time, and stigmas.19, 20 A stigma is an inaccurate belief against individuals based on a specific characteristic, race, or nation of people.22,23 Often, we see this in patients with a mental illness. Stigma towards individuals with SUDs also exist and are one of the most challenging barriers because of a misconception that an SUD is not a disease or medical condition and individuals with an SUD are at fault.23 You may hear people say, “They don’t want to get better” or “I don’t want those kinds of people in my pharmacy.” Stigmas can impede care and harm the patient.
It is important to recognize that an SUD is a medical condition and requires treatment. Stigmatizing language like “addict” or “junkie” has a negative connotation and can lead to barriers in care. Avoid using stigmatizing language. For example, an addiction is an SUD. Clinicians need to replace the words “addict” or “junkie” with the words “person with an SUD.” This recognizes the disease and not the person with the SUD.
Patient case Joe and brief intervention.
Joe is a 32-year-old man who hurt his back three years ago in a car accident. He has used opioids since the accident, but he still complains of pain. He supplements his medications by purchasing additional opioids online and on the street. Joe also has a history of alcohol use. He consumes three to four beers on most days. His family is concerned with his alcohol and drug use and recommends he seek help.
AUDIT score: 12-At risk use
DAST-10 score: 5-Harmful use
What recommendations are appropriate based on the screening results?
Joe’s alcohol screening score of 12 shows that he is at risk use and his DAST-10 score of 5 shows that his use of drugs is harmful. In Joe’s case, he would benefit from a brief intervention and referral to treatment.
A brief intervention would be helpful for Joe. Here is an example of an intervention between Joe and the pharmacist at the ambulatory care clinic.
Pharmacist: “Good morning, Joe. Would it be OK if I speak with you for a few minutes about your screening results that you took earlier?”
Joe: “I guess that would okay.”
Pharmacist: “Based on your screening results, your alcohol use puts you at risk for harm and your drug use is possibly already harmful for your health and for those around you.”
Joe: “I don’t know what you are talking about. I don’t have a problem.”
Pharmacist: “Let me ask you this. From your perspective what is your relationship with alcohol and drugs?”
Joe: “Well I guess I do drink every day and I am on oxycodone for the pain. I was in an accident a few years ago and the pain won’t go away. I need the oxy. My family thinks I need help.”
Pharmacist: “Thank you for opening up to me and telling me how you feel after your accident and that you’re still in pain. Tell me some of the things that are good about your alcohol and drug use and some things that are not good?”
Joe: “Well alcohol helps me forget about my problems for little bit. The drugs help my pain, but I feel guilty sometimes because I buy it off the street because my doctor won’t give me enough.”
Pharmacist: “What is it about your drug use that makes you feel guilty?”
Joe: “My family means a lot to me, and I am afraid that my wife might leave me and take the kids.”
Pharmacist: “It sounds like you love your family. What changes do you think you could make about your alcohol and drug use?”
Joe: “Well I guess I could cut back on my drinking and find some other ways to deal with my stress. I rely too much on the oxy so I don’t think I could cut back on that right now.”
Pharmacist: “That’s great that you are willing to cut back on your alcohol use. Tell me what that would look like?”
Joe: “I think I could limit myself to three beers a day instead of four or five. I can start there and see how it goes.”
Pharmacist: “That’s a great start. On a scale of 1-10 where 1 means that you are not at all ready to make this change and 10 meaning that you are completely ready where do you think you would put yourself on this scale?”
Joe: “I guess I would rate myself as being a 7.”
Pharmacist: “Joe, that’s great. A 7 is very close to being completely ready to make this change. Can I ask you what is holding you back from you being at a 10?
Joe: “I don’t think that I am completely ready to make a change. I am also afraid of failing.”
Pharmacist: That is a valid fear. Speaking with someone about your alcohol use and treatment can really help. Would you be willing to meet Dr. Smith here at the office and set up an appointment with him?”
Joe: “Sure. I could meet him now while I am at the clinic.”
The pharmacist walks Joe down the hall to meet Dr. Smith who is a behavioral specialist focusing on SUDs. The pharmacist performs a warm handoff, introducing Joe to Dr. Smith.
The pharmacist engaged Joe in the conversation and reflected on what Joe said and felt. During the conversation, the pharmacist asked open-ended questions to gain more insight into Joe’s alcohol and drug use and discussed his readiness to make a change. Joe rated himself as a 7 on the readiness scale. Discussing where they are on the readiness ruler can determine patients’ willingness to change, possible resistance, and potential fears. Joe recognized the pros and cons of his alcohol and drug use and made a plan to decrease his alcohol use and meet with a behavioral specialist about his drug use.
Conclusion
SBIRT is a public health approach to intervene with individuals at risk of an SUD. SBIRT is effective in reducing alcohol use by 40% and illicit drug use by 76%.24 Applying universal screening and promoting change to reduce high-risk behavior before it escalates to an SUD can greatly reduce patient harm and minimize healthcare costs.
Depending on the setting, time constraints, day-to-day workload, and staffing, SBIRT may be a challenge to perform. Pharmacists and pharmacy technicians should be knowledgeable about SBIRT and treat persons with SUDs, where feasible, in a professional, caring manner. SBIRT can be a useful approach to identify those with at risk behaviors and apply early intervention methods to minimize harm and development of an SUD.
Pharmacist Post Test (for viewing only)
SBIRT Exam Questions
Pharmacist
After completing this continuing education activity, pharmacists will be able to
1. Discuss the prevalence and consequences of SUDs
2. Describe the components of SBIRT
3. Recognize motivational interviewing skills to promote readiness to change
4. Discuss harm reduction and how it pertains to SUDs
5. Describe barriers associated with the use of SBIRT in the community setting
1. SBIRT is a public health approach to identify persons at risk of a substance use disorder. For the acronym SBIRT, what does BI stand for?
A. Brief Interaction
B. Brief Intervention
C. Brief Intermediation
2. In the U.S., which of the following substances is most abused?
A. Nicotine
B. Alcohol
C. Oxycodone
3. Which of the following is used to screen for alcohol use?
A. AUDIT
B. DAST
C. ADST
4. Jim, a 42-year-old man, completed the alcohol screening questionnaire and scored 17. How would you rate his alcohol use?
A. At-risk use
B. Harmful use
C. Dependent use
Use patient case Sean for questions 5-7.
Sean is 42-year-old male who presents to the emergency department after a car accident. He scores 14 on the AUDIT questionnaire and the pharmacist performs a BNI. He has not worked since COVID and drinks to forget about his problems. The pharmacist discusses Sean’s drinking habits and related harm. Sean is defensive and states that he does not have a drinking problem.
5. Which of the following is an appropriate response to Sean’s statement, that he does not have a drinking problem?
A. “It seems to me you have a drinking problem. That’s how you ended up in the hospital.”
B. “You need to stop drinking or this will happen again. I’ve seen it time and time again.”
C. “Can we talk more about how you ended up in the emergency department today?”
6. The pharmacist reflects on Sean’s statements. Which is one of the following is example of reflective listening?
A. “Let’s create an action plan to decrease your alcohol use so you can have some goals to accomplish.”
B. “ I know that you don’t want to be here today, but can you see how important it is?”
C. “Thank you for sharing how you feel about losing your job. That must be hard for you.”
7. The pharmacist wants more information about Sean’s motivation to change behavior. Which of the following promotes the BEST response?
A. “Are you willing to cut back on your alcohol use?”
B. “What are some negative effects of your alcohol use?”
C. “Do you think your alcohol use contributed to the car accident?”
8. Fill in the blank. Harm reduction involves policies, programs, and practices to focus on the individual’s ________ ________.
A. Substance Use
B. Harmful Behaviors
C. Human Rights
9. Which of the following is an example of non-stigmatizing language?
A. He has a substance use disorder
B. He is addicted to drugs
C. He is heroin junkie
10. Which of the following is a barrier to providing SBIRT in a community pharmacy setting?
A. Cost of screening
B. Safety
C. Stigmas
Pharmacy Technician Post Test (for viewing only)
Pharmacy Technician Post-test
After completing this continuing education activity, pharmacist technicians will be able to
1. Discuss the prevalence and consequences of SUDs
2. Describe the components of SBIRT
3. Discuss harm reduction and how it pertains to SUDs
4. Describe barriers associated with the use of SBIRT in the community setting
1. SBIRT is a public health approach to identify persons at risk of a substance use disorder. For the acronym SBIRT, what does BI stand for?
A. Brief Interaction
B. Brief Intervention
C. Brief Intermediation
2. In the U.S., which of the following substances is most abused?
A. Nicotine
B. Alcohol
C. Oxycodone
3. Which of the following is used to screen for alcohol use?
A. AUDIT
B. DAST
C. ADST
4. Which of the following is an example of non-stigmatizing language?
A. He has a substance use disorder
B. He is addicted to drugs
C. He wants to be a junkie
5. Which of the following is associated with the distribution of clean needles/syringes?
A. Reduction of blood borne diseases
B. Increase in illicit drug use
C. Increase in drug overdoses
6. What are the recommended alcohol drinking limits for men who are younger than 65 years?
A. No more than 1 drink per day and no more than 7 drinks per week
B. No more than 2 drinks per day and no more 14 drinks per week
C. No more than 4 drinks per day and no more than 14 drinks per week
7. Which of the following is used to screen for drug use?
A. AUDIT
B. DAST
C. ADST
8. What is the goal of harm reduction?
A. Keeping people safe
B. Stopping drug use
C. Giving people free needles
9. Which of the following is a barrier to providing care to those with a SUD in a community pharmacy setting?
A. Cost of screening
B. Safety
C. Stigmas
10. SBIRT is effective in reducing alcohol use by___ %
A. 40%
B. 76%
C. 20%
References
Full List of References
References
1. Substance abuse and mental health services administration. 2017 NSDUH annual national report. Accessed June 9, 2021. Available at https://www.samhsa.gov/data/report/2017-nsduh-annual-national-report
2. Centers for Disease Control and Prevention. Excessive Drinking is Draining the U.S. Economy. Updated December 2019. Accessed June 21, 2021. https://www.cdc.gov/features/costsofdrinking/
3. National Drug Intelligence Center. National Drug Threat Assessment. Washington, DC: United States Department of Justice; 2011. Accessed June 21, 2021. www.justice.gov/archive/ndic/pubs44/44849/44849p.pdf
4. Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal Costs of Prescription Opioid Abuse, Dependence, and Misuse in the United States. Pain Medicine. 2011; 12:657-667.
5. Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction. 2003; b;98(9):1209–1228.
6. Institute of Medicine (IOM). Broadening the base of treatment for alcohol problems. Washington, DC: National Academies Press; 1990.
7. Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Subst Abuse. 2007;28(3):7–30.
8. Shonesy BC, Williams D, Simmons D, Dorval E, Gitlow S, Gustin RM. Screening, Brief Intervention, and Referral to Treatment (SBIRT) in a retail pharmacy setting: The pharmacist’s role in identifying and addressing risk of substance use disorder. J Addict Med. 2019; 13(5):403-407.
9. WHO screening and AUDIT. Accessed June 9, 2021. http://www.who.int/substance_abuse/activities/sbi/en/
10. Smith PC, Schmidt SM, Allensworth-Davies D eta. A single-question screening test for drug use in primary care. Arch Intern Med. 2010; 170(13):1155−1160.
11. Centers for Disease Control and Prevention. Alcohol use and your health. Accessed June 9, 2021. Available at: http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm
12. National Institute of Alcohol Abuse and Alcoholism (NIAAA) for alcohol. Accessed June 9, 2021. Available at https://www.rethinkingdrinking.niaaa.nih.gov/how-much-is-too-much/is-your-drinking-pattern-risky/Drinking-Levels.aspx.
13. Miller WR, Moyers TB. Motivational Interviewing and the clinical science of Carl Rogers. J Consult Clin Psychol. 2017; 85(8):757-766. doi: 10.1037/ccp0000179.
14. Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13:39–46.
15. Miller WR, Rollnick S. Motivational Interviewing: Helping people to change (3rd Edition). Guilford Press; 2013.
16. Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism. Accessed June 9, 2021. Available at https://www.motivationalinterviewing.org/sites/default/files/MATCH.pdf
17. Substance Abuse and Mental Health Services Administration. Behavioral health treatment services. Accessed August 2, 2021. Available at https://findtreatment.samhsa.gov/
18. Harm reduction international. Accessed July 7, 2021. Available at https://www.hri.global/what-is-harm-reduction.
19. Hawk KF, Vaca FE, D'Onofrio G. Reducing fatal opioid overdose: Prevention, treatment and harm reduction strategies. Yale J of Biol and Med 2015;88(3):235–245.
20. Werremeyer A, Mosher S, Eukel H, et al. Pharmacists’ stigma toward patients engaged in opioid misuse: When “social distance” does not mean disease prevention. [published online ahead of print, 2021 March 22]. Subst Abuse. 2021;Mar 22; 1-8. doi: 10.1080/08897077.2021.1900988
21. Murphy A, Phelan H, Haslam S, Martin-Misener R, Kutcher SP, Gardner DM. Community pharmacists’ experiences in mental illness and addictions care: a qualitative study. Subst Abuse Treat, Prev, and Policy. 2016; 11:6 DOI 10.1186/s13011-016-0050-
22. Caddell J, Gans S. Verywellmind. What is stigma? Accessed August 5, 2021. Available at https://www.verywellmind.com/mental-illness-and-stigma-2337677
23. Fernandez L. Addiction or Substance Use Disorder? How Using the Right Language Helps Fight Stigma. Accessed August 12, 2021. Available at https://illuminaterecovery.com/blog/substance-use-disorder-stigma/
24. Aldridge A, Linford R, Bray J. Substance use outcomes of patients served by a large US implementation of Screening, Brief Intervention and Referral to Treatment (SBIRT). Addiction. 2017; Feb; 112 (Suppl. 2), 43–53 doi: 10.1111/add.13651.