Learning Objectives
After completing this application-based continuing education activity, pharmacists and pharmacy technicians will be able to
- Differentiate systemic approaches to medication errors and individual (personal) responsibilities for medication errors
- Outline various causes for medications errors that can be traced back to individuals
- Discuss how unique work habits influence the propensity to make errors
- Apply methods to reduce an individual’s medication error rate

Release Date:
Release Date: May 1, 2023
Expiration Date: May 1, 2026
Course Fee
Pharmacists: $7
Pharmacy Technicians: $4
There is no grant funding for this CE activity
ACPE UANs
Pharmacist: 0009-0000-23-016-H05-P
Pharmacy Technician: 0009-0000-23-016-H05-T
Session Codes
Pharmacist: 23YC16-XVK33
Pharmacy Technician: 23YC16-TXP82
Accreditation Hours
2.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-23-016-H05-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
Amanda Choi, PharmD
Pharmacist
Backus Hospital
Norwich, CT
Carren Jepchumba, PharmD
Pharmacy Manager
Kroger Health
Indianapolis, IN
Jeannette Wick, RPh, MBA, FASCP
Dir. Office of Pharmacy Professional Development
UConn School of Pharmacy
Storrs, CT
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Drs. Choi and Jepchumba and Ms. Wick have no relationships with ineligible companies and therefore have nothing to disclose.
ABSTRACT
Pharmacists and pharmacy technicians must be careful not to make
errors, but errors slip through from time to time. Organizations (healthcare systems,
hospitals, and pharmacies) often use systems-based approaches to error
prevention. Pharmacy employees need to know about systems-based approaches,
but they also need to know about approaches they can use themselves to reduce
their own chances of error. This activity describes factors that increase the
likelihood of error and methods that are proven to help individuals focus. We
discuss–and strongly recommend–knowing your limit, tracking and recording errors,
collaborating with coworkers, employing tools that increase accuracy, and
stopping the workflow when things “feel” wrong.
CONTENT
Content
INTRODUCTION
Pharmacists and pharmacy technicians strive to provide safe, high-quality care to people when they are unwell, but sometimes we make errors. No one likes to make an error, and in our field, errors can have devastating consequences: preventable illness and injury, unnecessary hospitalizations, disability, and sometimes even death. Experts who have extrapolated data indicate that medical errors now account for 9.5% of all deaths in the United States, which if true, would make medical mistakes the third leading cause of death after heart disease and cancer.1
Addressing issues systemically has become commonplace in healthcare systems. Most of us know that the first step in resolving medication errors is being able to identify where errors occur and factors that contribute to their occurrence. Tracking in this way allows us to integrate preventive measures into our systems and habits to reduce future occurrence. It’s also important to create safe workplace environments so individuals involved in errors are not afraid to address future errors.2
But external factors aren’t the sole cause of medication errors. Psychosocial and cognitive factors can seriously impact the rates at which errors occur. Individuals who identify their own habits or knowledge gaps that might contribute to errors can take the next step: working on improving.
Definitions of “Medication Error”
To identify and prevent medication errors properly, having a clear, unambiguous definition would be ideal. Unfortunately, everyone seems to use similar—but different—definitions. Each person has a role and individual actions impact the team’s overall performance. Let’s compare a few definitions:
An error is a failure to complete a planned action as intended or the use of an incorrect plan of action to achieve a specific endpoint. Bad judgment, ignorance, or inattention might cause this type of error. A pharmacy situation might be when a technician fails to remove expired, very expensive medication and order new stock. When a new patient is admitted to the hospital and needs the medication immediately, the pharmacist hurries to process the order. Assuming that all medication in stock is in-date, the pharmacist approves an intravenous (IV) bag. At final verification, the pharmacist finally notices the medication’s expiration date. With no in-date stock, the pharmacist cannot send the IV. This mistake disrupts patient care. The pharmacy technician failed to keep the inventory in-date and the pharmacist assumed, failed to pay attention, and didn’t double check before proceeding.
An error is the enactment of a misconception due to incorrect information or part of a statement that is incorrect. An example in pharmacy might be when a doctor sends a new prescription with a higher-than-expected quantity, fails to update the prescription signatura (sig) or instructions, but tells the patient to take a higher dose. The puzzled pharmacist proceeds to process it. The insurance rejects the claim highlighting the calculated days-supply did not match the quantity indicated. While the pharmacist works on the prescription, the patient comes to the pharmacy to pick up her prescription. The pharmacist cannot contact the doctor who wrote the prescription and the doctor’s colleagues cannot confirm the prescription because they are unsure. The pharmacist decides to dispense a lower quantity per the old instructions so that the insurance will approve it. With the prescription now approved, the pharmacist dispenses the prescription but because the patient follows the doctor’s verbal directions, she runs out sooner than indicated on the prescription. She returns a few days later demanding more. The patient must now contact the insurance, the doctor, and the pharmacist to obtain the prescription that she needs. This could have been avoided if the doctor had noted that the patient would be taking the same drug at an increased dose.
An error is the departure from what is ethically acceptable or an incorrect result produced by automation. As healthcare systems increase their use of electronic health records, this problem is increasing. Most systems are programmed to increase efficiency with the autofill function—meaning the computer will fill a field automatically based on the most common entry—which can increase avoidable errors. Too often, healthcare personnel blindly accept the computer-generated entry or calculations. This can result in a patient being given too much or too little drug and disrupt the quality of care.
In summary, medication errors occur in many ways (see Table 1). When a medication error occurs, it reduces the chances of achieving a desired outcome and the margin of safety associated with that outcome. Some medication errors result in adverse drug reactions but many do not. This is because not all adverse events cause adverse drug reactions.3 Many of us have made errors that serendipitously improved something. For example, a person making carrot soup may misread the words “1 garlic clove” and “1 teaspoon of cloves.” The soup will be different—and possibly better—than if the cook used garlic cloves. In medicine, however, errors are rarely “Happy Accidents” and we need to make every effort to reduce and eliminate them.
Table 1. Definition of Medication Errors
- A misconception resulting from incorrect information
- A wrong action attributable to bad judgment or ignorance or inattention
- Departure from what is ethically acceptable
- Inadvertent incorrectness
- Part of a statement that is not correct
- The occurrence of an incorrect result produced by a computer
- Unintentional failures to act or plan (when it’s intentional, it’s a violation, not an error)
Source: Reference 3
Systemic Failures: Avoiding Blame
Many healthcare systems and providers now stress approaches that analyze errors as systemic failures. Systems, by nature, are interrelated units that work together toward the same goal. Most medication errors occur as a result of multiple, compounding events—or collapse of a faulty system—rather than an individual’s isolated act.4,5 It’s amazing how many times a serious error occurs because employees missed the opportunity to catch and rectify an error at multiple points in the patient’s care. Using a systems approach4,6
- avoids assigning blame
- explores relationships between various parts of the system, and
- recognizes that cause and effect may be separated by space or time.
Many experts describe systemic failure using a Swiss cheese analogy. The holes in Swiss cheese represent the faults within a system. If an error passes through one of the holes in one slice of Swiss cheese, one would hope that the holes of the next slice of cheese won’t align, blocking the error. If the holes of the Swiss cheese slices all align, that medication error would slip through and reach the patient. Recognizing the placement of each slice—or the placement of each healthcare professional and that professional’s responsibility to be vigilant—can decrease the likeliness that a medication error will occur and it’s also key in identifying systemic failures.7,8
This Swiss cheese analogy can be applied to community pharmacy, where pharmacy staff establish multiple checkpoints during the filling process to ensure prescriptions are filled correctly (reviewing, scanning barcodes, tablet appearance, etc.). However, many patient safety cultures tend to look for explanatory causes for trouble and encourage blaming, criticizing, or silencing healthcare providers who make errors.4 For this reason, some experts refer to the individual who makes an error as the “second victim.” Lack of support from colleagues and supervisors can greatly affect involved health care providers’ ability to cope, leading to greater distress or protracted recovery.9
Fears of blame and punishment can deter individuals from reporting their errors, which can prevent creation of a culture of safety. Admitting one’s mistakes allows open discussion with peers and performance improvement experts can prevent further patient harm if they identify and fix the systemic “hole” causing the mistake.2,4 Let’s look at systems-based approaches first, and then examine why individual approaches are also critical.
QUALITY AND PERFORMANCE IMPROVEMENT APPROACHES
Various workplaces take different approaches to errors, but risk managers have proven certain approaches are more successful than others (see Table 2). The two most common approaches to analyzing medication errors are tracking and trending. Almost every workplace, whether it’s a healthcare facility or some other kind of business—requires employees to complete incident reports if they make an error. A responsible individual (usually someone designated as a quality or performance improvement specialist or a risk manager, although individuals may be interested in looking at their own errors) should look at incident reports over time to determine
- What type of error or errors are most common
- If a particular drug or product is involved in multiple incidents and why
- The time of day or workload volume when the error occurred
- The individual or individuals involved
This amounts to a type of detective work, in which the responsible party investigates medication errors individually and collectively to track and trend predisposing factors. If the data indicates that certain factors are trending (occurring more than once), the workplace can take action to prevent the error from happening again.10 Sometimes the action is as simple as heightening employees’ awareness that errors have occurred. Other times, the workplace might place a sign on a shelf indicating that a product is a look-alike or sound-alike product, mark bottles with bright colors to differentiate them, use TALL man lettering (see SIDEBAR), or conduct training so staff is better educated.
SIDEBAR; What is TALL man Lettering?
TALL man lettering is the practice of writing part of a drug's name in upper case letters to help distinguish sound-alike, look-alike drugs from one another. The goal is to differentiate drug names visually and avoid medication errors. The Office of Generic Drugs of the U.S. Food and Drug Administration (FDA) encourages manufacturers to use TALL man lettering labels. Many hospitals, clinics, and health care systems use TALL man lettering in their computerized order entry, automated dispensing machines, medication admission records, prescription labels, and drug product labels. Does your system use TALL man lettering? If not, should it?
The Institute for Safe Medication Practices creates a list of TALL man lettering for drug names. Most—but not all—of the drugs on the list are generic products. Find the list here: https://www.ismp.org/recommendations/tall-man-letters-list.
Here’s a snapshot from the center of the list:
| Drug Name with TALL Man Letters | Confused with |
| hydrALAZINE | hydrOXYzine – HYDROmorphone |
| HYDROmorphone | hydrOXYzine – hydrALAZINE |
| hydrOXYzine | hydrALAZINE – HYDROmorphone |
| medroxyPROGESTERone | methylPREDNISolone – methylTESTOSTERone |
| methylPREDNISolone | medroxyPROGESTERone – methylTESTOSTERone |
| methylTESTOSTERone | medroxyPROGESTERone – methylPREDNISolone |
| mitoXANTRONE | Not specified |
| niCARdipine | NIFEdipine |
| NIFEdipine | niCARdipine |
| prednisoLONE | predniSONE |
| predniSONE | prednisoLONE |
| risperiDONE | rOPINIRole |
| rOPINIRole | risperiDONE |
Source: Reference 11
Table 2. Common Approaches to Medication Error-Related Performance Improvement
| Term | Definition |
| Tracking | · The ability to assess performance; following the course or trail of someone or something, usually to find them or note their location. In pharmacy, this could include:
|
| Trending | · Monitoring the general direction in which something is developing or changing. In pharmacy, monitoring has led to expansion of the pharmacists’ role. Examples include vaccination administration, collaborative practice agreements in certain states, tobacco cessation programs, and point-of-care testing.
· A method of estimating future costs of health services by reviewing past trends in cost and utilization of those services. |
| Root cause analysis | · A full investigation of the causes of unexpected events followed by identification and implementation of appropriate and effective strategies to prevent similar occurrence in the future.
· Asking “Why?” until it cannot be answered, often employing a “fishbone diagram” that looks at potential issues with materials, machines, methods, environment, measurements, and people. · It helps pharmacies take a process-driven, system-based approach to address errors. |
| Workplace re-engineering | · Planned elimination, addition, or distribution of functions or duties in the workplace focused on innovative strategies to develop leaders, engage employees, and foster healthy workplace culture.
· Is often influenced by excessive or insufficient labor, poor patient outcomes, or political or economic changes. |
| Disaster drill or mock code | · An exercise or demonstration that tests the readiness and capacity of a hospital, a community, or other systems to respond to a possible public health emergency or other disaster. |
Source: References 12, 13, 14, 15, 16, 19
In the event a serious error occurs, workplaces need to go beyond simple steps. One such step is to conduct a root cause analysis (RCA). RCA starts by reviewing what and how an event occurred, and expands the investigation to identify why it happened. Many organizations explain to their employees that RCA is the art of asking “Why” until no more questions beginning with “Why” are possible. Armed with that information, the RCA team can develop workable corrective measures that prevent future events of the type observed. RCA is not flawless, but it ensures that teams of people look at very serious errors and develop approaches that could prevent them in the future.20
Finally, errors are more likely to occur when unusual, unexpected, or unanticipated situations arise. For this reason, many organizations run disaster drills and observe them closely. In this way, they can identify areas where their systems are weak and implement corrective measures.21
Successful Programs
To create the best possible error prevention program, organizations can look at what has been proven to work. It’s clear that behavior-based programs create better outcomes than technology or any other approach.4 A leading researcher in pharmacy error identified six elements common to the most effective behavior-based programs (See Figure 1).4
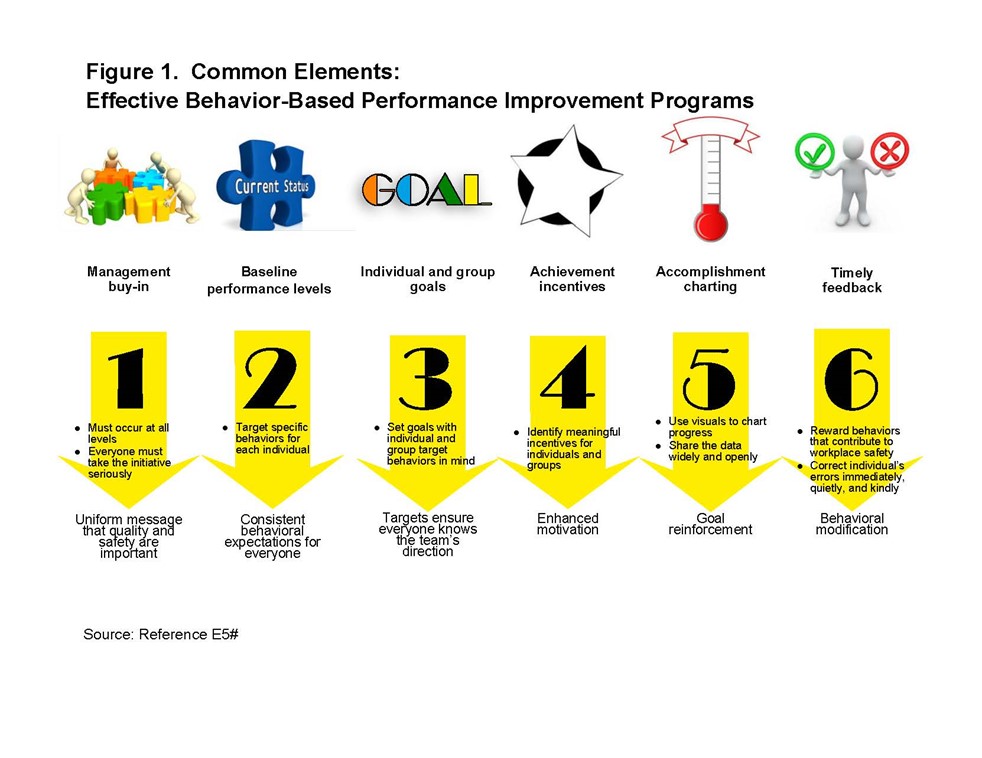
Efforts that address the system and the individual jointly and individually are prudent. Consider a systemic safety measure: the widespread use of technology that is “smart.” Relying on technology and assuming it never fails may make some individuals become complacent and less vigilant until it is too late.4 Examples in community pharmacy are automated inventory systems and bar-code scanners. A person who enters data into a system—this would be an employee in the inventory management section in most pharmacies or healthcare systems—has a slight chance of entering an incorrect drug name. If no one catches the error, the last chance to prevent an error rests with the pharmacist who verifies that the tablet matches the description in the system before it is dispensed to the patient. The final check—a step that cannot and must not be automated—is an individual responsibility. Taking the extra seconds to verify the drug (while remembering that sometimes technology fails) can save a patient’s life from what could have been a deadly mistake.4
Many psychosocial factors also influence work performance. Work-as-imagined (work that is anticipated and described in official policies and procedures compiled by administrators or policy makers) and work-as-done (the way that employees actually accomplish work) are often quite different.22 Factors associated with the process of filling prescriptions are shown in Table 3.
Table 3. Psychosocial Factors that Influence Work Performance
- Anxiety or depression
- Changing workload
- Competing tasks
- Determination to “get the job done” despite barriers
- Distraction or interruption
- Hurrying
- Insufficient decision support
- Insufficient staffing
- Knowledge gaps
- Lack of experience
- Lack of non-technical skills training (examples include communication, decision-making, reasoning, team work, time management)
- Machinery or hardware that is difficult to operate
- Perception that an error could lead to criminal charges
- Rapidly changing or evolving roles
- Use of “work-arounds” (shortcuts or approaches that differ from procedure) to overcome barriers
- Vague or incomplete policy or procedure
Source: References 6, 22, 23, 24
The physical environment (inadequate illumination, environmental distractions, and noise), interruptions in workflow, facility design, technology, poorly designed labels, interpersonal relationships (e.g., number of interfaces with people and the level of stress and conflict caused by those interactions), and workload can adversely affect accuracy. 25,26,27
Many pharmacy employees associate high workload with increased error rates. They are often surprised to learn that low-workload conditions are more closely linked with errors than high-workload conditions. Consider a study conducted in 2000 that involved pharmacists, pharmacy technicians, and 21,672 prescriptions. Pharmacy employees made more process errors under low-workload conditions (11.2%) than under high-workload conditions (6.1%) and during periods when the workload trended downward in volume (at the start of a shift or after a break).28,29 In general, pharmacists were more vulnerable to mistakes when processing fewer than 15 prescriptions per hour than when processing more than 25 prescriptions per hour. (Author aside: We include these numbers because the study reported them, not as a hard and fast rule. We acknowledge that everyone has unique working habits, and some people can feel burned out processing fewer prescriptions than others.) A little bit of task tension (from perceived workload) seemed to result in fewer errors while filling prescriptions. However, there may be limits to the increases in task tension that would provide desirable results—too much stress and tension can become a problem. Overall, low levels of objective workload and subjective task tension were associated with more errors.26,30
Personal qualities can also play a role. Impulsivity, task frustration, fatigue, perceptual ability, concern for doing well, a lack of physical hardiness, and magnitude of personal effort expended can cause more errors to progress through the verification process unnoticed. Individuals should examine their task-related anxiety and overall job-related depression (a strong predictor of overall job stress often manifesting as constant complaining at work, impatience with coworkers, the need for “mental health days,” difficulty getting up on workdays, or physical illnesses) and address them if possible. Supervisors should examine employees’ task-related anxiety and overall job-related depression to help individuals cope; if not, anxiety and depression will affect job satisfaction and performance.4,22
Workplace support is also an important factor and the study mentioned earlier also demonstrated its importance. Pharmacists who had supervisors who they perceived as helping them set task goals and gain appropriate autonomy made fewer errors. Pharmacists who had supervisors who were overly autocratic (meaning domineering or overly involved in supervision) experienced tension that interfered with dispensing prescriptions accurately. Pharmacists who believed the number of breaks they receive was adequate to meet their needs made fewer process errors. 26 Later studies also confirm that poor leadership and insufficient support can adversely influence accuracy.22
ERRORS: WHAT WE KNOW
Errors are inevitable, but we must be able to recognize when we are prone to making errors to be able to limit them. Everyone has periods of increased errors—for instance during dramatic shifts in workload. Entering the pharmacy during peak hours can be stressful and predispose some individuals more than others to make errors they wouldn’t usually make. When we are flustered, our sense of logic escapes us momentarily.4,26
Some individuals make more frequent or predictable errors than others because of different cognitive styles. A classic study found that pharmacists whose cognitive styles include attention to details made fewer errors. It also found that about 12% of pharmacists have difficulty attending to details, and that 12% of pharmacists made 33% of errors.26 By using high-intensity task lights, exaggerated product label names (labels that are large and multicolored), NDC numbers, and specially designed devices for holding prescriptions at eye level during data entry, pharmacy staff who had difficulty being attentive to details made fewer errors.26 An 1999 incident monitoring study found poor communication and failure to check medical records when questions arose also contributed to errors.31 A more recent PRIORITIZE study conducted between September 2013 and November 2014 involving 500 North West London primary care clinicians noted the top three problems relating to medication errors in primary care were incomplete medication reconciliation during transitions of care, inadequate patient education about medication use, and poor discharge instructions.32 Clearly, healthcare providers have some communication problems.
A patient case in Pennsylvania illustrates the alarming consequences of poor communication between healthcare providers and fewer medication reconciliations. The patient was first hospitalized for uncontrolled blood pressure and acute kidney injury. At the time of discharge, one of her prescription medications was Norvasc® (a high blood pressure medication). The patient experienced worsening fatigue, slow movements, personality changes, and a ‘stoic’ facial expression with suboptimal blood pressure control. Soon after, she was hospitalized the second time for chest pain and underwent angioplasty. Several weeks later, she was diagnosed with anxiety and depression and was prescribed prescription medications for these conditions. The patient was admitted a third time to the emergency room after a fall with light-headedness and poor ambulation. It was only at the third visit when the medication reconciliation team realized her outpatient pharmacy accidentally dispensed Navane® (generic name as thiothixene, an antipsychotic) instead of Norvasc®. When thiothixene was discontinued, her clinical status improved. This preventable medication error occurred because the pharmacy staff and physician deemed the written prescription legible, when in actuality, it was not.8
Typically, people make mistakes or slips most frequently when new to the profession and lacking experience. A long period during which mistakes are rare follows. Eventually everyone develops unique work habits, and error rates tend to increase again, usually as bad habits develop.29,33
Finally, humans work on autopilot around 80% of the time. This means that 80% of the time, we don’t fully register what we are doing in our brain; we don’t engage with the task at hand and instead just go through the motions. Pharmacists also have an “inner pharmacist” who should kick in and take them out of autopilot mode when issues out of the ordinary arise.30,34,35 Often, when faced with errors after-the-fact, we clearly recall the circumstances under which they occurred because we wake up from our autopilot. We’ll talk more about autopiloting below.
How People Work
Workload in the pharmacy has been traditionally measured as the number of prescriptions dispensed per hour or day, or the number of prescriptions dispensed per pharmacist. Experts predict that the typical pharmacist’s workload has and will increase for two reasons:
- An increase in demand from an aging population and
- The addition of pharmacist-provided services (examples include medication therapy management, helping women select oral contraceptives in some states, and immunizations).
Instead of only focusing on the numbers, pharmacists, pharmacy technicians, and the organizations that employ them should focus on understanding the individual’s subjective experience of work demands. For pharmacists, verifying patient’s information, performing patient consultation and drug utilization reviews, and verifying prescriptions for accuracy can be demanding to the point that high workload negatively impacts performance. For technicians, similar factors—performing repetitive and mundane tasks, expanding roles, and high-risk assignments—may increase stress or create situations in which they must multi-task. Understanding that work is a process and not a series of discrete events can help maintain the “big picture.”30 That big picture is that pharmacists and pharmacy technicians must promote patient safety; dispensing to keep up with the pharmacy queue—the people who are in line or who have called in—is not prudent.36
Over the course of the day, filling many prescriptions is bound to cause a person go on autopilot—which is understandable. Humans are creatures of habit and routine. All humans work on autopilot around 80% of the time.4,34,35 Autopiloting occurs when the brain recognizes a situation and rapidly selects appropriate responses using familiar, predictable behavior context. The brain does this to preserve energy. Essentially, we perform most tasks reasonably well without thinking much about them. Many readers will sigh with recognition when they read this example: many people have left home on a non-work day to go someplace that’s in the general direction of work. They may be surprised to find themselves in their workplace’s parking lot. That’s autopilot. In the retail setting, pharmacy technicians and pharmacists autopilot the most when they are dealing with insurance coding and billing to third-party insurers. Autopiloting is usually safe.37
Our autopiloting should stop when we encounter stressful situations that are unfamiliar because our brains don’t know how to react appropriately in unfamiliar situations. In stressful situations, we tend to misapply familiar rules and knowledge. Intense emotion blocks out our sense of logic. In these situations, we have to remember to exercise mindfulness—taking a little bit of time away from the regular work stream to assess the situation calmly and proceed with a plan of action.4
It’s also crucial for each worker to know his or her own tendency to make errors and do what is necessary to refocus.4 However, all pharmacy employees must recognize that some people’s propensities and capabilities are hardwired.33 They cannot change their abilities and will approach work the same compulsive way, regardless of training.
Using technology to help us work is effective, but technology has limitations.38 Technology makes us lazy and unfamiliar with manual processes that have been automated. It is common for individuals to become complacent because we believe a machine designed for a specific purpose will complete the task correctly for us. We tend to trust that technology will work well all the time. It doesn’t.39 For instance, refilling a carousel cassette with the wrong medication will not prevent the machine from filling the prescription. This error can go undetected unless the pharmacist performs a final check before dispensing to the patient. This emphasizes the importance of the pharmacist’s individual responsibility as mentioned earlier.4,39
Self-improvement
While all of us prefer not to make errors, expecting an error rate of zero is unreasonable.4 Errors will happen. As noted above, some people make more errors than others, and a landmark study found that 12% of pharmacists made 30% of reported errors.26 Certainly, we all work with others who seem to make a disproportionate share of the workplace’s errors, and those who seem to be remarkably accurate. Where do you fall on the spectrum?
Examining your own error rate requires insight. This term—insight—is used most often in psychiatry and is defined as the patient’s awareness and understanding of the origins and meaning of his or her attitudes, feelings, and behavior, and disturbing symptoms.40 It means understanding of oneself. It has a slightly different meaning in the context of medication errors. In problem solving, it means the sudden perception of the appropriate relationships between things that results in a solution.41,42
Some people, and especially those who are error-prone, have poor insight. It may result from fixation, over-reliance on experience and past circumstances, rushing to solve a problem, or using the same approach over and over and expecting different results. Let’s look at each of these individually.
Fixation error refers to the tendency for the brain’s perceptual field to narrow and shorten in a crisis.43,44 When this happens, we develop a sometimes stymieing compulsion to fixate on the problem we think we can solve, and ignore almost everything else. During periods of fixation, time becomes distorted; minutes often seem longer than usual. In addition, the fixated individual may not hear input from others. Even the most skilled and experienced professionals can develop a fixation in periods of high stress.43,44
An example is that of a stalled car stuck on a level crossing as a distant train barrels toward it. The driver starts and restarts the engine, when the best way to save his life is to exit the car and run. In pharmacy, fixation errors occur when the provider concentrates on a single aspect of a case or problem to the detriment of other more relevant aspects. To break out of a fixation, individuals must be able to recognize the demand for a new approach to the problem and to produce a solution that works. Individuals who tend to fixate need to learn to43,44
- Ask themselves what is different about the current problem
- Heighten awareness of the people around them and listen
- Invite others into the problem solving team to identify alternatives
Over-reliance on experience and past circumstances often occurs during emergencies. In this case, the individual tends to rely on past experience (even if it doesn’t apply in the current situation), and have difficulty abandoning assumptions based on that experience. In short, the person applies incident-specific experience to a situation that is probably much broader in nature. An example would be investigating why a patient who has asthma is experiencing exacerbations. If the pharmacist assumes the problem is treatment nonadherence when the actual problem is that the inhaler is faulty or requires skills like visual acuity or manual dexterity that the patient does not possess, the assumption can be deadly. In addition, during emergencies, individuals may have trouble recalling information accurately (elevated cortisol levels tend to change cognition and thinking). Often, using a cognitive aid like a checklist, decision tree, or an algorithm can help clarify thinking and lead to faster—and better—solutions.45
It’s interesting that many pharmacy staff members say, “I was rushing,” when they analyze errors, but few studies looked at or identified rushing as a cause. Rushing to problem-solve can increase the likelihood of error. An older study found that physicians linked 10% of errors to rushing or fatigue.31 Experts in medication error science also indicate that rushing contributes to error.46 An older study in Canada looked at a pilot program that transferred order entry responsibilities from pharmacists to pharmacy technicians. At the end of the study, the error rate had increased from 2.5% to 6%. Analysis indicated that technicians were rushing to enter orders, and re-training technicians to slow down and be mindful reduced the error rate to below the baseline level.47 Often, technicians may try to fill more quickly, or pharmacists rush the final verification step of dispensing as the customer line lengthens, and errors occur.
One area of growing interest is interruptions and interruption management.48,49 Interruptions have been shown to increase the medication error rate, and some studies suggest a technique called interruption management. They suggest using a “do not interrupt” sign or even a piece of clothing that warns people to stay away until the healthcare professional completes the task. They also recommend using a checklist for multistep processes. At this time, it’s unclear if these interventions help.48,49
Finally, many of us have fallen victim to a common dilemma: using the same approach over and over and expecting different results.4 Healthcare practitioners as a rule, do many tasks—even complicated ones—from memory rather than from following a checklist. Over time, and especially when we see our error rates beginning to climb upward, it’s important to look at our own work and consider ways in which we need to adjust or change (see Table 4). We cannot rely on what we did before. Over time, people change, workplaces change, and many of the problem’s underlying elements change.4 As we analyze errors, we must include what we’ve learned in the past, but be open to fresh approaches and ideas.
Table 4. Improving Your Own Accuracy
| Do this…. | And then do this… |
| Periodically review your errors and near-misses. | Analyze errors to determine if you see a trend like confusing look-alike, sound-alike or spell-alike drugs.
Determine if you can take steps to reduce the likelihood of a similar error happening again. Develop and use checklists if errors occur in multi-step processes. |
| Schedule visual and hearing exams more frequently as you age. | Wear appropriate glasses or hearing aids at work.
Ask your employer for assistive devices (supplemental lighting, a magnifier, or a phone amplifier), or secure these yourself. |
| Solicit feedback from peers and supervisors about ways to reduce your own and others’ errors. | Maintain a quiet, composed demeanor in the workplace. |
| Address workplace distractions as soon as you become aware of them. | Reduce noise and clutter, improve lighting. |
| Understand technology’s limitations. | Maintain your skills so that if technology fails, you can revert to the pre-technology work method. |
| Value relationships with coworkers and promote good organizational dynamics. | Resolve disputes immediately, and retire grudges.
Provide feedback to coworkers constructively. |
| Address developing personal problems (alcohol abuse, marital discord) early.
|
Engage with your employer’s employee assistance program before your supervisor refers you. |
| Understand that some people make errors because they lack knowledge. | Address your own knowledge gaps, and promote a culture of learning. |
| Avoid relying on “workplace re-engineering” or “work task design” to prevent errors; these may fail as the workplace composition and focus changes. | Learn to engage and listen to your “inner pharmacist” or “inner technician” when something is out of the ordinary.
|
When we discuss medication errors, it’s critical to talk about data entry errors because they represent about 25% of all medication errors.25 The pharmacy has many repetitive tasks like data entry or filling prescriptions. Many of these tasks can be completed without conscious awareness. This ‘autopilot’ function contributes to data entry errors like misspellings or errors recorded on the patient’s profile. The vast majority of data entry errors are inconsequential, but some are dangerous.25
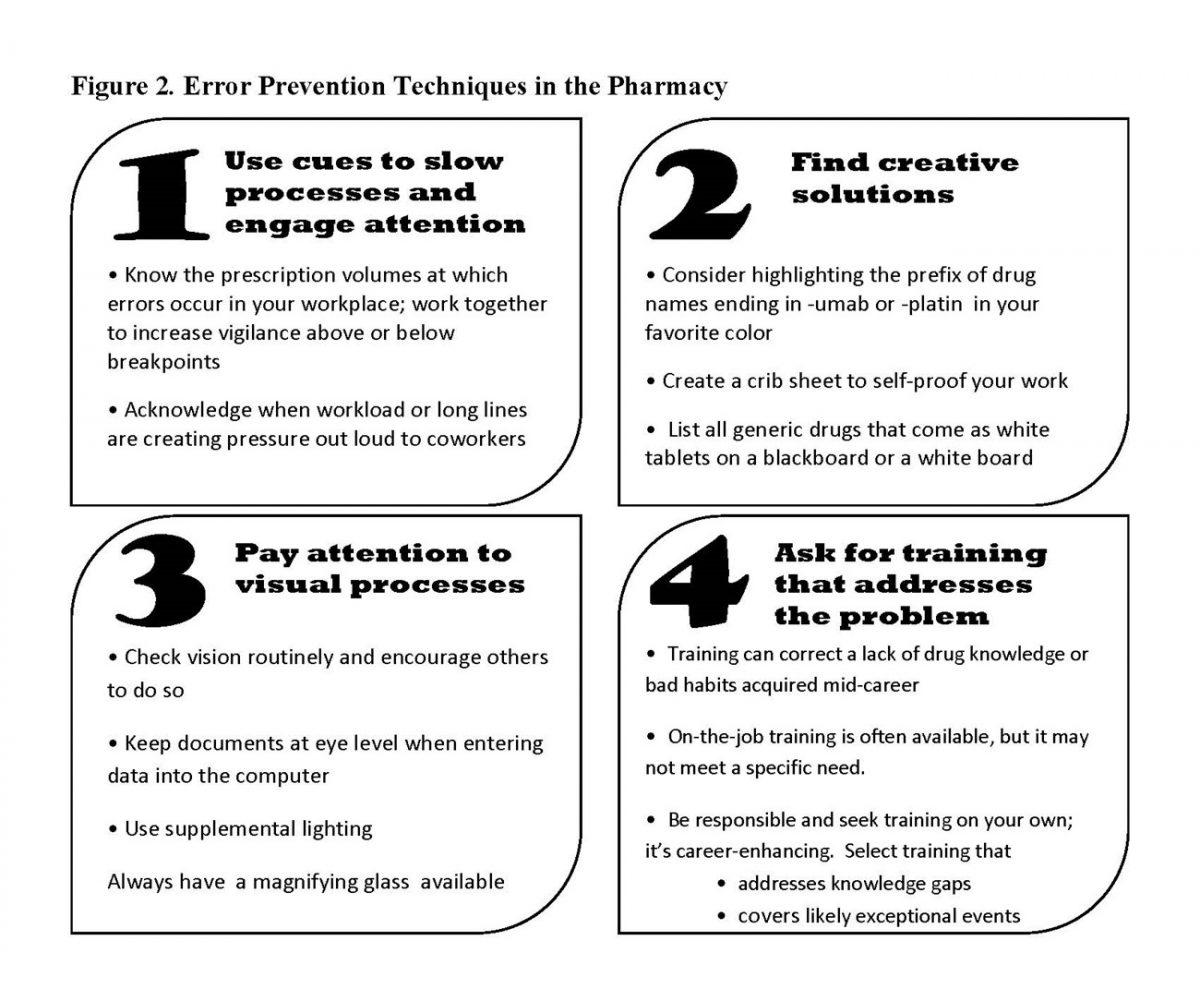
Many factors could impact the cognitive system directly. Pharmacists and pharmacy technicians can take some simple steps to increase accuracy in the pharmacy. Figure 2 suggests a few, but individuals will find the best solutions are those they develop themselves and tailor to their own habits and circumstances.
Reducing Workplace Turbulence
Workplace turbulence occurs when something causes discomfort or decreases workplace stability. Some things that cause workplace turbulence include poor temperature control (it’s either too hot or too cold), noise, clutter, uncertainty, or working with people who have different styles or personalities that are abrasive to you. These things affect accuracy and productivity. If workplace distractions are the problem, making small changes to decrease turbulence can make large differences.29,33
If the problems are environmental, ask the appropriate person to help resolve them. Establishing good relationships with the people who provide environmental support—people in building supervision, maintenance, and housekeeping—is imperative. They can often help adjust the ambient temperature or reduce clutter. Learning to work with instead of against or parallel to coworkers and supervisors can improve the environment.4 The key is telling your supervisor how you best hear constructive criticism and delivering constructive criticism to others in a positive way—and in the way they receive it best.
Finally, be aware of when you are fatigued or unable to perform at your peak and enlist coworkers' help by asking them to monitor your work.29,33
Poka-Yoke
Since the 1960s, many industries have adopted the principles of poka-yoke, also called “mistake-proofing,” to prevent errors.50 Poka-yoke is a systems approach, but unlike many systems approaches, the people closest to the work (not administrators or policy makers) propose the action. Defined broadly, poka-yoke refers to any behavior-shaping constraint in a process that prevents faulty behaviors by the worker. An industrial engineer at Toyota developed this concept, and it encourages workplaces to look at common mistakes and develop processes that make it impossible for workers to make the mistake in the future. Basically, it’s defensive workplace design. It depends on involving the people closest to the work to identify what to mistake-proof and develop ideas to prevent very specific mistakes. In pharmacies, four poka-yoke principles are used often, and can be applied in many more areas.50-52
First, workplace managers need to empower employees to pause or even stop the work process entirely if they believe that an error is in process.29 Employees need to be able to ask four questions respectfully:
- Did we do everything?
- Did we do everything right?
- Does it look, sound and feel right?
- Are these our usual work conditions?
Next, everyone in the pharmacy community from manufacturers to distributors to providers who work in direct patient care need to make it easier for people to do the right thing than the wrong thing. A short example can clarify this principle. Years ago at the National Cancer Institute, a collaborating company was developing a new monoclonal antibody (MAB). The MAB was lyophilized and came in a fairly large multidose vial. It needed to be reconstituted with 20 mL of a specific diluent. The manufacturer provided the MAB with a vial of the diluent that contained 30 mL. The astute reader will see the potential for error. In many cases, pharmacists and pharmacy technicians who worked in investigational drug preparation looked at the package, and simply transferred the diluent—all 30 mL of it—into the larger vial. The resultant solution was an incorrect dose. Can you see why? Diluting a 400 mg vial with 20 mL creates a 20 mg/mL solution. Using 30 mL creates a 13.33 mg/mL solution. After investigational drug employees identified and reported this error several times, and the NCI reported it to the manufacturer, the simple poka-yoke fix was implemented. Although it took quite some time to implement the change, eventually the manufacturer packaged the MAB with a vial of diluent that had the correct amount needed in it—20 mL.
People who work in pharmacy in any capacity can make it easier to do the right thing than the wrong thing in numerous ways. Let’s discuss four of them.
- Putting items that will always be used together in that same container, and making sure that the items that are assembled are the correct sizes or doses or quantities, is kitting at work. It results in fewer missing parts, and it also speeds your process. Some experts estimate that it can cut errors by as much as 80%.53 The solution noted above is an example of kitting. Other examples of kitting are creating bowel evacuation kits for patients having colonoscopies, or assembling packages of items that are frequently prescribed together for specific procedures or treatments.
- Keying simply means that a process can’t be started without a key or tool of some sort. The requirement to remove your ATM card before receiving cash is an application of this principle so people don’t leave their cards in the machine. An example in the pharmacy is a computer that requires the user to insert an ID card to start the system. This increases accuracy and prevents users from signing in early in the day, walking away from the computer, and allowing others to operate under an incorrect sign-in code. Another example of a type of keying is moving pseudoephedrine to behind the counter in the pharmacy. Adding that step—requiring customers to sign for pseudoephedrine and limiting quantities—ensures there is a check in the process. States that have implemented this step have decreased the amount of pseudoephedrine diverted to methamphetamine production significantly.
- Interlocking uses simple mechanisms so that parts will only fit with other appropriate pieces. These are simple, low cost devices that prevent parts from being assembled incorrectly. An everyday example of poka-yoke for someone who always forgets or loses his keys is to place the keys in the shoes he will wear tomorrow. An example in pharmacy might be providing drugs meant to be administered intrathecally in a device that cannot attach to any intravenous equipment.
- Tell-tales let you know when you have made an error. Barcoding is a type of telltale. When you scan a barcode and it doesn’t match the barcode on the actual order, it sends you an alert that you’ve made an error.
The last poke yoke principle we’ll cover is this: Make mistakes obvious to workers immediately and discretely so they can make on-the-spot corrections, and allow people to take corrective actions or stop the work flow before irreversible damage is done. This small kindness brings errors to the error-maker’s attention, and allows immediate learning.
CONCLUSION
Despite our best intentions, some errors escape the confines of the pharmacy. Randomly checking completed work that has apparently passed verification sometimes identifies problem areas. But, some errors are just that—unfortunate events that could not be anticipated and occurred due to a confluence of factors. Even though reaching a medication error rate of zero is improbable, we should still make efforts to acknowledge our professional responsibility in our own work habits. Creating solutions tailored to our habits and circumstances can help reduce error rates and encourage a focus on a workplace culture of patient safety—not the number of prescriptions filled—as the big picture in pharmacy.
Pharmacist Post Test (for viewing only)
LEARNING OBJECTIVES
After participating in this activity, pharmacists and pharmacy technicians will be able to:
1. Discuss the difference between systemic approaches to medication errors and individual (personal) responsibilities for medication errors
2. Outline various causes for medications errors that can be traced back to individuals
3. Discuss ways in which peoples’ unique work habits influence their propensity to make errors
4. Identify methods to reduce an individual’s medication error rate and apply them appropriately
1. Which of these can INCREASE the chance of making errors?
A. Labeling of common look-alike, sound-alike drugs on shelves
B. Working on autopilot to perform tasks that are very routine
C. Working during a dramatic increase or decrease in workload
2. Which is an example of individual responsibility for medication errors?
A. A hospital administration implements autofill functions in the computer software to improve efficiency
B. A pharmacist provides the final check of a prescription after the prescription bottle comes out of the carousel
C. A manufacturer packages an intramuscular injection and its diluent in proper quantities in the same box
3. Eloise is a pharmacist at your hospital pharmacy. She is a reliable employee and one of the most skilled and experienced members of the pharmacy team. She has good recollection, even in stressful situations, but she tends to fixate when dealing with emergencies. If this situation occurs, which of the following should she perform FIRST?
A. Isolate herself from the people around her so she can think
B. Try to rectify the problem based on her past experiences
C. Take a moment to ask herself what’s different about this problem
4. What have studies of errors in healthcare found to be TRUE?
A. Eventually everyone’s error rate increases after a period of time working in their profession.
B. Addressing the system and individual jointly and individually is useless for analyzing errors.
C. Technology creates better outcomes than behavior-based programs.
5. What was the cause of the medication error in the Pennsylvania patient case described in this CE activity?
A. Poor communication
B. Bad work habits
B. Autopiloting
6. Which one of these is an example of how can individuals can improve their personal medication error rates?
A. Using the same approach over and over for different situations for consistency
B. Pointing out other team members’ mistakes so others will not do the same thing
C. Applying what you know works well while being open to fresh approaches and ideas
7. Mike is a pharmacy technician who works in a community retail pharmacy. He prides himself on being a people-person and receiving good feedback from patients. Last month while chatting with customers, he accidentally reconstituted an antibiotic medication with too much diluent. The pharmacist dispensed it and the patient now has a resistant infection due to receiving suboptimal treatment. As the pharmacist filled out an incident report, he told ML to stop talking with the customers and focus on his work. Since then, ML has become quieter. Patients have noticed his change in demeanor and brought it up with the pharmacist. What do you think the pharmacist should do next?
A. Tell patients that nothing’s wrong with Mike. He’s just focusing on his work because he made an error when he was distracted previously.
B. Ask Mike if he has a moment to talk about last week’s incident, apologize, to him and ask how Mike would prefer to hear criticism in the future.
C. Disregard their concerns – Mike was a chatter box who needed to learn how to limit his talking sooner rather than later.
8. Which of the following statements describe how the workload in the pharmacy should be measured?
A. The number of prescriptions per hour or day
B. The individual’s subjective experience of work demands
C. The number of prescriptions per pharmacist
9. CJ is an experienced pharmacist. With a growing number of tasks, CJ has been struggling to stay afloat. On a busy afternoon, CJ administered multiple immunizations and answered dozens of phone calls. The wait time was longer and longer. CJ made a list of his remaining tasks. He decides to rush through prescriptions to clear the queue. Which of the following could contribute to increased risk of medication error and is within CJ’s control?
A. The growing list of tasks to be done as a pharmacist
B. A particularly busy work day or time of day at the pharmacy
C. Rushing without addressing ways to readjust to accommodate for new tasks
10. Which factors help reduce medication error?
A. Leaving conflicts in the workplace unresolved and unacknowledged
B. Avoiding personal problems until they become a problem at the work place
C. Creating a safe environment for individuals involved in the error
11. Which of the following is a cognitive factor that influences workplace performance?
A. Changing workload
B. Insufficient staffing
C. Attention to detail
12. Which is an example of a SYSTEMIC approach that would increase medication errors?
A. A pharmacist performs final verification of a prescription after final packaging
B. The pharmacy implements automated inventory systems, autofill, and bar code scanners
C. A technician carefully checks for expiration dates and disposes medication accordingly
13. Which of the following would INCREASE an individual’s medication error rate?
A. Relying on technology whenever possible and utilize more “smart technology”
B. Maintaining skills so that if technology fails, you can revert to manual work methods
C. Wearing appropriate glasses, secure assistive devices or hearing aids at work.
14. Which of the following will INCREASE medication errors that are traced back to individuals?
A. Employees routinely examine their task-related anxiety and job-related depression
B. The pharmacy has poor leadership and insufficient support for employees
C. Pharmacy employees believe the number of breaks they receive are adequate
Pharmacy Technician Post Test (for viewing only)
LEARNING OBJECTIVES
After participating in this activity, pharmacists and pharmacy technicians will be able to:
1. Discuss the difference between systemic approaches to medication errors and individual (personal) responsibilities for medication errors
2. Outline various causes for medications errors that can be traced back to individuals
3. Discuss ways in which peoples’ unique work habits influence their propensity to make errors
4. Identify methods to reduce an individual’s medication error rate and apply them appropriately
1. Which of these can INCREASE the chance of making errors?
A. Labeling of common look-alike, sound-alike drugs on shelves
B. Working on autopilot to perform tasks that are very routine
C. Working during a dramatic increase or decrease in workload
2. Which is an example of individual responsibility for medication errors?
A. A hospital administration implements autofill functions in the computer software to improve efficiency
B. A pharmacist provides the final check of a prescription after the prescription bottle comes out of the carousel
C. A manufacturer packages an intramuscular injection and its diluent in proper quantities in the same box
3. Eloise is a pharmacist at your hospital pharmacy. She is a reliable employee and one of the most skilled and experienced members of the pharmacy team. She has good recollection, even in stressful situations, but she tends to fixate when dealing with emergencies. If this situation occurs, which of the following should she perform FIRST?
A. Isolate herself from the people around her so she can think
B. Try to rectify the problem based on her past experiences
C. Take a moment to ask herself what’s different about this problem
4. What have studies of errors in healthcare found to be TRUE?
A. Eventually everyone’s error rate increases after a period of time working in their profession.
B. Addressing the system and individual jointly and individually is useless for analyzing errors.
C. Technology creates better outcomes than behavior-based programs.
5. What was the cause of the medication error in the Pennsylvania patient case described in this CE activity?
A. Poor communication
B. Bad work habits
B. Autopiloting
6. Which one of these is an example of how can individuals can improve their personal medication error rates?
A. Using the same approach over and over for different situations for consistency
B. Pointing out other team members’ mistakes so others will not do the same thing
C. Applying what you know works well while being open to fresh approaches and ideas
7. Mike is a pharmacy technician who works in a community retail pharmacy. He prides himself on being a people-person and receiving good feedback from patients. Last month while chatting with customers, he accidentally reconstituted an antibiotic medication with too much diluent. The pharmacist dispensed it and the patient now has a resistant infection due to receiving suboptimal treatment. As the pharmacist filled out an incident report, he told ML to stop talking with the customers and focus on his work. Since then, ML has become quieter. Patients have noticed his change in demeanor and brought it up with the pharmacist. What do you think the pharmacist should do next?
A. Tell patients that nothing’s wrong with Mike. He’s just focusing on his work because he made an error when he was distracted previously.
B. Ask Mike if he has a moment to talk about last week’s incident, apologize, to him and ask how Mike would prefer to hear criticism in the future.
C. Disregard their concerns – Mike was a chatter box who needed to learn how to limit his talking sooner rather than later.
8. Which of the following statements describe how the workload in the pharmacy should be measured?
A. The number of prescriptions per hour or day
B. The individual’s subjective experience of work demands
C. The number of prescriptions per pharmacist
9. CJ is an experienced pharmacist. With a growing number of tasks, CJ has been struggling to stay afloat. On a busy afternoon, CJ administered multiple immunizations and answered dozens of phone calls. The wait time was longer and longer. CJ made a list of his remaining tasks. He decides to rush through prescriptions to clear the queue. Which of the following could contribute to increased risk of medication error and is within CJ’s control?
A. The growing list of tasks to be done as a pharmacist
B. A particularly busy work day or time of day at the pharmacy
C. Rushing without addressing ways to readjust to accommodate for new tasks
10. Which factors help reduce medication error?
A. Leaving conflicts in the workplace unresolved and unacknowledged
B. Avoiding personal problems until they become a problem at the work place
C. Creating a safe environment for individuals involved in the error
11. Which of the following is a cognitive factor that influences workplace performance?
A. Changing workload
B. Insufficient staffing
C. Attention to detail
12. Which is an example of a SYSTEMIC approach that would increase medication errors?
A. A pharmacist performs final verification of a prescription after final packaging
B. The pharmacy implements automated inventory systems, autofill, and bar code scanners
C. A technician carefully checks for expiration dates and disposes medication accordingly
13. Which of the following would INCREASE an individual’s medication error rate?
A. Relying on technology whenever possible and utilize more “smart technology”
B. Maintaining skills so that if technology fails, you can revert to manual work methods
C. Wearing appropriate glasses, secure assistive devices or hearing aids at work.
14. Which of the following will INCREASE medication errors that are traced back to individuals?
A. Employees routinely examine their task-related anxiety and job-related depression
B. The pharmacy has poor leadership and insufficient support for employees
C. Pharmacy employees believe the number of breaks they receive are adequate
References
Full List of References
References
- Anderson JG, Abrahamson K. Your health care may kill you: medical errors. Building Capacity for Health Informatics in the Future. 234:13-17. DOI 10.3233/978-1-61499-742-9-13. Accessed December 27, 2022. http://ebooks.iospress.nl/publication/46132.
- Rogers EE, Griffin E, Carnie W, et al. A just culture approach to managing medication errors. Hosp Pharm. 2017;52(4):308-315.
- Aronson, J. (2019). Medication errors: definitions and classification. Accessed December 27, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2723196/
- Grasha AF. Into the abyss: seven principles for identifying the causes of and preventing human erros in complex systems. Am J Health-Syst Pharm. 2000:57:544-564.
- Hodgson BB, Kizior RJ. Appendix L. In: Hodgson BB, Kizior RJ, Saunders Nursing Drug Handbook 2013. 1st edition. St. Louis, Missouri, Saunders/Elsevier; 2012:1290.
- Vosper H, Lim R, Knight C, et al. Considering human factors and developing systems- thinking behaviours to ensure patient safety. Clinical Pharmacist. 2018,10:2. Accessed December 27, 2022. https://dspace.lboro.ac.uk/dspace-jspui/bitstream/2134/28474/3/Hignett_Vosper%202018%20ACCEPTED%20%20pharmaceutical-journal.com.pdf
- Rosen RK. Medication errors: a 21st-century perspective. Proceedings (Bayl Univ. Med Cent). 2004;17(4):464-467;discussion 467-468.
- da Silva BA, Krishnamurthy M. The alarming reality of medication error: a patient case and review of Pennsylvania and National data. J Community Hosp Intern Med Perspect. 2016;6(4):31758.
- Quillivan RR, Burlison JD, Browne EK, et al. Patient safety culture and the second victim phenomenon: connecting culture to staff distress in nurses. Jt Comm J Qual Patient Saf. 2016:42(8):377-86.
- Rogers, Erin, et al. A Just Culture Approach to Managing Medication Errors. National Center for Biotechnology Information, April 2017. Accessed December 27, 2022. www.ncbi.nlm.nih.gov/pmc/articles/PMC5424837/
- Institute for Safe Medication Practices. Look-alike drug names with recommended tall man letters. Accessed December 27, 2022.Available at https://www.ismp.org/recommendations/tall-man-letters-list
- “Emergency Preparedness: 3 Steps to Prepare Your Pharmacy.” PBA Health, 12 Mar. 2018, Accessed December 27, 2022. Emergency Preparedness: 3 Steps to Prepare Your Pharmacy (pbahealth.com)
- Reorganization. Defined Term. Accessed December 27, 2022. https://definedterm.com/reorganization
- Root Cause Analysis Workbook for Community/Ambulatory Pharmacy. Institute For Safe Medication Practices. Accessed December 27, 2022. www.ismp.org/resources/root-cause-analysis-workbook-community-ambulatory
- Schwartz, Heidi. Re-Engineering the Workplace For Employee Wellness. January 26, 2015. Facility Executive Magazine. Accessed December 27, 2022. https://facilityexecutive.com/2015/01/employers-will-be-challenged-to-re-engineer-the-workplace-attract-and-retain-people/
- “Tracking.” Defined Term. Accessed December 27, 2022. https://definedterm.com/tracking
- Benedetto AR. Six Sigma: not for the faint of heart. Radiol Manage. 2003;25(2):40-53.
- Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 4, 2022.
- “Trending.” Defined Term. Accessed December 27, 2022. https://definedterm.com/trending
- Agency for Healthcare Research and Quality. Root cause analysis. Accessed December 27, 2022. https://psnet.ahrq.gov/primers/primer/10/root-cause-analysis
- “Lessons We Don't Learn: A Study of the Lessons of Disasters, Why We Repeat Them, and How We Can Learn Them.” January 15, 2015. HOMELAND SECURITY AFFAIRS. Accessed December 27, 2022. www.hsaj.org/articles/167
- Sutherland A, Ashcroft DM, Phipps DL. Exploring the human factors of prescribing errors in paediatric intensive care units. Arch Dis Child. 2019;104(6):588-595. doi:10.1136/archdischild-2018-315981
- Bhangu A, Bhangu S, Stevenson J, Bowley DM. Lessons for surgeons in the final moments of Air France Flight 447. World J Surg. 2013;37(6):1185-1192.
- Croft H, Nesbitt K, Rasiah R, Levett-Jones T, Gilligan C. Safe dispensing in community pharmacies: applying the software, hardware, environment and liveware (SHEL) model. Pharmaceutical J. 2017;9(7): DOI: 10.1211/CP.2017.20202919. Accessed December 27, 2022. https://www.pharmaceutical-journal.com/research/safe-dispensing-in-community-pharmacies-applying-the-software-hardware-environment-and-liveware-shell-model/20202919.article
- Grasha AF, Schell K. Psychosocial factors, workload, and human error in a simulated pharmacy dispensing task. Perceptual Motor Skills. 2001;92:53-71.
- Grasha AF. Understanding medication errors: a cognitive systems approach. Medscape. May 14, 2001. Accessed December 27, 2022. https://www.medscape.org/viewarticle/418538
- Grasha AF, Reilley S, Schell K, Tranum D, Filburn J. A cognitive systems perspective on human performance in the pharmacy: implications for accuracy, effectiveness, and job satisfaction. Cincinnati, Ohio: University of Cincinnati,2000, Cognitive Systems Lab Report 062100-R.
- Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention. ADE Prevention Study Group. JAMA. 1995;274(1):29-34.
- Barry R, Murcko AC, Brubaker CE. The Six Sigma Book for Healthcare. Ann Arbor, MI: Chicago Health Administration Press; 2002:19-43.
- Grasha AF. Misconceptions about pharmacy workload. Can Pharmaceut J. 2001;134(4):26-35.
- Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust. 1999;170(6):287-288.
- Tudor CL, Papachristou N, Gallagher J, et al. Identifications of priorities for improvement of medication safety in primary care: a PRIORTIZE study. BMC Fam Pract. 2016;17(1):160.
- Bogner MS. Misadventures in Healthcare. Mahwah, NJ: Lawrence Erlbaum Associates; 2004:1-186
- Ashcraft MH. Human memory and cognition (2nd ed.). New York: Harper Collins, 1994.
- Anderson JR. Learning and memory: An integrated approach. New York: John Wiley & Sons, 1995.
- Chui MA, Mott DA. Community pharmacists’ subjective workload and perceived task performance: a human factors approach. J Am Pharm Assoc (2003). 2012;52(6):e153-e160.
- Vatansever D, Menon DK, Stamatakis EA. Default mode contributions to automated information processing. PNAS. 2017;114(48):12821-12826.
- Gouraud J, Delorme A, Berberian B. Autopilot, mind wandering, and the out of the loop performance problem. Front Neurosci. 2017;11:541.
- Casey S. Set Phasers on Stun: And Other True Tales of Design, Technology and Human Error. Santa Barbara, CA: Aegean; 1998.
- “Insight,” The Free Dictionary. Accessed December 27, 2022. https://medical-dictionary.thefreedictionary.com/insight
- Psychestudy. Insight Learning. Accessed December 27, 2022. https://www.psychestudy.com/behavioral/learning-memory/insight-learning
- How to Detect Insight Moments in Problem Solving Experiments. Accessed December 27, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5854655/
- Fioratou E, Flin R, Glavin R. No simple fix for fixation errors: cognitive processes and their clinical applications. Anaesthesia. 2010;65(1):61-69.
- Leslie I. How mistakes can save lives: one man’s mission to revolutionise the NHS. June 4, 2014. Accessed December 27, 2022. https://www.newstatesman.com/2014/05/how-mistakes-can-save-lives
- Jenkins B. Cognitive aids: time for a change? Anaesthesia. 2014;69:655–668.
- Grasha AF. Tools for the reflective practitioner: Using self-monitoring, personal feedback and goal setting to reduce error. Health Notes Qual Assur. 2002;19-24.
- Tierney M, McLurg D, Macmillan C. Transferring medication order entry from pharmacists to pharmacy technicians. JCPH. 1999;52(4):240-243.
- Lapkin S, Levett-Jones T, Chenoweth L, Johnson M. The effectiveness of interventions designed to reduce medication administration errors: a synthesis of findings from systematic reviews. J Nurs Manag. 2016;24(7):845-858. doi:10.1111/jonm.12390
- Castro-Rodríguez C, De Lucas-Volle S, González-Roca I, Diaz-Redondo A, Mora-Capín A, Marañón R. Professionals' Perception of a Strategy to Avoid Interruptions During Medication Handling. J Patient Saf. 2023;19(1):29-35. doi:10.1097/PTS.0000000000001082
- Soliman-Junior, J., Tzortzopoulos, P., and Kagioglou, M. 2020. “Exploring Mistakeproofing in Healthcare Design.” In: Tommelein, I.D. and Daniel, E. (eds.). Proc. 28th Annual Conference of the International Group for Lean Construction (IGLC28), Berkeley, California, USA, doi.org/10.24928/2020/0034
- Van Scyoc K. Process safety improvement--quality and target zero. J Hazard Mater. 2008;159(1):42-48.
- Kumar S, Steinebach M. Eliminating US hospital medical errors. Int J Health Care Qual Assur. 2008;21(5):444-471.
- China Manufacturing Consultants. 6 Poka Yoke (mistake proofing) techniques that most factories overlook. Accessed December 22, 2022. http://www.cmc-consultants.com/blog/6-poka-yoke-mistake-proofing-techniques-that-most-factories-overlook