Learning Objectives
After completing this application-based continuing education activity, pharmacists will be able to:
- DESCRIBE common pathways through which pets are exposed to toxic human medications
- IDENTIFY the clinical signs and symptoms of toxicity from antidepressants, ADHD medications, NSAIDs, opioids, and recreational drugs in companion animals
- DISCUSS veterinary management strategies and outcomes for pets exposed to toxic medications, including decontamination, symptom management, and diagnostic testing
- RECOGNIZE best practices to counsel pet-owning patients on safe medication storage, disposal, and early signs of pet poisoning
After completing this application-based continuing education activity, pharmacy technicians will be able to:
- RECOGNIZE common human medications that are toxic to pets
- IDENTIFY signs and symptoms of drug toxicity in companion animals that may be mentioned by pet owners at the pharmacy counter
- LIST proper techniques for medication storage and disposal that can reduce the risk of pet exposure
- RECOGNIZE when to refer pet-owning patients to the pharmacist for counseling or poison control center guidance

Release Date
Release Date: January 15, 2026
Expiration Date: January 15, 2029
Course Fee
Pharmacists $7
Pharmacy Technicians $4
There is no funding for this CE.
ACPE UANs
Pharmacist: 0009-0000-26-001-H05-P
Pharmacy Technician: 0009-0000-26-001-H05-T
Session Codes
Pharmacist: 26YC01-NZQ39
Pharmacy Technician: 26YC01-QNZ93
Accreditation Hours
2.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-26-001-H05-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
Brianna Champagne, B.S. Pharmacy Studies
Recent graduate of the University of Connecticut Medical Writing Certificate program
Storrs, CT
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Brianna Champagne has no relationships with ineligible companies.
ABSTRACT
Medications are the leading cause of toxic exposure in household pets (cats and dogs), surpassing traditional hazards like chocolate or household cleaners. As prescriptions for antidepressants, attention-deficit/hyperactivity disorder (ADHD) medications, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and recreational drugs increase nationwide, so does the risk to companion animals. Pharmacists and pharmacy technicians—often on the front lines of medication safety—can educate pet-owning patients on how to prevent accidental poisonings and recognize early signs of toxicity. This continuing education activity provides an overview of the most dangerous drug classes for cats and dogs, including clinical symptoms, treatment strategies, and emerging trends in veterinary toxicology. It also explores ethical and legal concerns, such as reporting obligations and the growing need for pet-safe medication packaging. Participants will gain evidence-based tools to support safe medication use in homes with animals and strengthen their role in harm prevention and patient education.
CONTENT
Content
INTRODUCTION
Pharmacists and pharmacy technicians often think of medication safety in terms of human patients, families, and caregivers. But what about their pets? Companion animals are increasingly victims of preventable medication poisoning. Many of these cases start with a dropped pill, an open purse, or a topical patch worn on the skin.
According to the American Society for the Prevention of Cruelty to Animals (ASPCA) Animal Poison Control Center (APCC), prescription and over-the-counter (OTC) drugs are in the top three causes of pet toxicities reported each year. OTC medications were reported as #1, accounting for 16.5% of all exposures, and human prescription medications as #3. Human food and drinks are at #2, with 16.1% of exposures.1 This trend shouldn’t be surprising. Many homes contain a wide array of medications, increasing the risk of accidental pet exposure.2 Our environments are filled with substances that can be fatal to a curious cat or an aimless labrador.
Since 2020, pet ownership in the United States (U.S.) has surged. According to the American Pet Products Association, nearly 70% of U.S. households now own at least one pet.3 As medication safety educators, pharmacists are increasingly expected to support patients as pet owners, not just as individuals. Technicians, too, often serve as the first line of communication at the pharmacy counter. Pharmacy employees might wonder, "But how am I supposed to help? I don’t treat animals." Pharmacy teams don’t have to treat animals. Pharmacy employees’ jobs include protecting the whole household—including pets. That means
- Educating pet-owning patients about safe storage and disposal
- Recognizing red flags during patient conversations
- Referring to the correct veterinary resources when exposure is suspected
Veterinarians can’t be the only line of defense. Poisonings can happen at home, where nearly every room poses a risk.4 By the time a pet reaches the animal hospital, irreversible damage may have already occurred. Pharmacy professionals are positioned to intervene upstream, at the point of medication access.
HIDDEN RISKS AT HOME
Pets are curious by nature. Their attraction to novel smells, crinkling containers, or flavored suspensions often leads to unintentional ingestion. If a patient says, "My dog ate my pills, but it was only a few," how would a responsible, educated pharmacy employee respond? Many pharmacy professionals would hesitate. It's easy to assume that exposure is rare or that a small amount won't matter. But the reality is that pets are exposed to human drugs every day, often in ways humans don’t think about. Understanding the routes of exposure helps pharmacy professionals anticipate risk and educate patients more effectively. Below are the three most common ways pets come into contact with toxic medications.
Direct Ingestion
This is the most well-known route—and often the most severe due to immediate high exposure.4 Examples include
- A pill falls on the floor and the pet swallows it before the owner notices
- A dog chews through a medication bottle, blister pack, or weekly organizer
- A cat licks liquid formulations left on a countertop
It’s reasonable to wonder, "Wouldn’t a dog spit out a bitter-tasting pill?" (like most do when given their own pills). Not necessarily. Dogs may chew through plastic out of boredom, and some drugs (like venlafaxine [Effexor] or amphetamine/dextroamphetamine [Adderall] tablets) have sweeteners or coatings that make them more palatable.
Secondary Exposure
Pets may lick topical medications—like estrogen creams or lidocaine patches—directly from human skin. This route is especially dangerous because it often happens without anyone noticing. For example, if a patient applies a lidocaine patch and then holds her pet for an hour, the pet could absorb significant amounts of the drug. This could happen transdermally or orally if the pet grooms after exposure.5
Toxic exposure is not only a problem for pets—it’s a problem for children. According to a review of adverse event reports collected by the Swedish Medical Products Agency, children experienced serious health effects after contact with transdermal hormone-containing products. Documented symptoms include precocious (early) puberty, accelerated growth, unresolved virilization, and female infertility.5 These cases highlight the need for better public awareness and clearer instructions for storage and use to protect pets and children.
PRO TIP: When patients pick up topical or transdermal medications, ask, "Do you have pets or children at home that come into contact with your skin or laundry?" If the answer is yes, explain the risk and recommend covering the treated area or changing clothes before interacting with pets and children. A 20-second conversation might prevent a life-threatening exposure.
Environmental Contamination
Improperly discarded medications or drug-laced household waste can lead to inhalation or ingestion of drug residues by pets. Trash scavenging is common—pets often ingest discarded medications, wrappers, or even tissues soaked in drug residue.4 Some medications are excreted in urine or feces; pets that drink from the toilet may be exposed. Pharmacy technicians can help here. During OTC purchases or casual conversations, technicians may hear, "My dog gets into everything!" That’s a red flag that indicates it’s time to include a pharmacist and educate the pet owner on trash safety, sealed storage, and disposal. Never assume a drug is pet-safe unless it has a veterinary-approved label.
PAUSE AND PONDER: How would you explain the difference between a pet’s metabolism and a human’s?
LOW DOSE, HIGH RISK
Small doses that are safe for humans can be dangerous for pets due to differences in size, metabolism, and enzyme activity. Doses of ibuprofen exceeding 250 mg/kg of body weight can cause gastric ulcers or kidney failure in a small dog or cat.6
Let’s break it down7-9
- Researchers develop flat dosing for medications for humans. But most cats and dogs weigh a fraction of the average human weight. A 10 lb dog or 8 lb cat might receive a lethal dose from licking a coated tablet. Sustained-release medications can remain in an animal’s system far longer than in a human’s, causing extended toxicity.
- Pets sometimes lack the enzymes humans rely on. Specifically, cats lack glucuronyl transferase—an enzyme essential to eliminate NSAIDs, acetaminophen, and opioids—making them highly susceptible to toxicity. Studies show that dogs often excrete a portion of certain drugs—such as NSAIDs and extended-release formulations—in the feces unchanged. This highlights pets’ limited ability to metabolize and eliminate these substances compared to humans. Both species have different gastric pH levels and gut flora that can affect absorption and breakdown.
Counseling should address two things. First, the pharmacist should explain that pets process medications differently than humans. Second, when accidental poisonings occur, pet owners should call a veterinary poison control hotline. They have veterinarians on staff around the clock and can determine if the dose the pet consumed is dangerous. The ASPCA APCC and Pet Poison Helpline are excellent, reliable resources. These calls often prevent unnecessary vet visits and guide lifesaving intervention when minutes matter.10 The SIDEBAR provides contact information for these resources.
SIDEBAR: Animal-specific Poison Control Centers
Human poison control centers do not manage veterinary cases. Instead, pharmacy teams and pet owners should be aware of the following specialized services.10
|
|
| Phone: 1-888-426-4435 | |
| Website: www.aspca.org/apcc | |
| Available 24/7; staffed by veterinary toxicologists | |
| Fee: $95 per case (covers phone consultation and follow-up) | |
|
|
| Phone: 1-855-764-7661 | |
| Website: www.petpoisonhelpline.com | |
| Available 24/7; includes licensed veterinarians | |
| Fee: $89 per case (includes updates to the attending veterinarian) | |
These hotlines charge a fee because they don’t receive government funding like human poison centers do. The cost supports rapid access to board-certified veterinary toxicologists and real-time risk assessments. After the client/pet owner pays for the consultation and the poison control specialist creates a case number, there are no further costs for following up on the case. The poison control center will work with the customer and a veterinarian until the case is resolved.10 In many cases, a single call can mean the difference between a $90 consultation and a $3,000 emergency vet bill.
TOP OFFENDERS
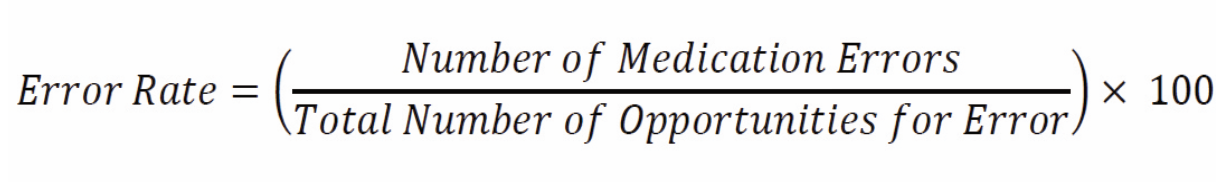
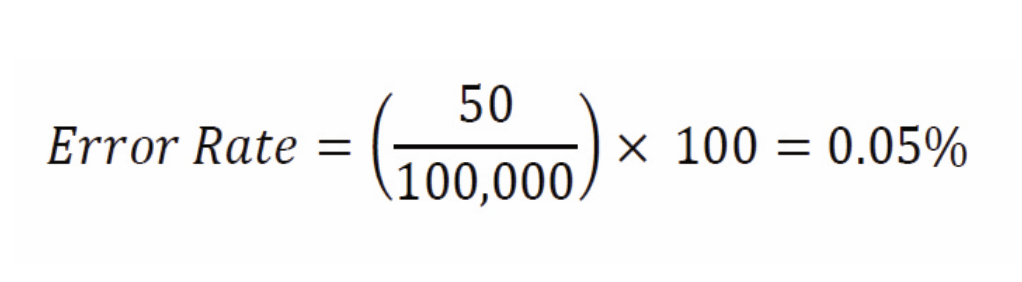
In veterinary toxicology, several drug classes account for most pet poisoning cases reported to animal poison control centers every year. Table 1 describes the five categories that are critical to know and how to recognize when a pet may be at risk.2,11,12
Table 1. Impact of Common Drug Poisonings on Pets6,11,13-15
| Medication Type | Common Symptoms |
| ADHD medications (amphetamine/dextroamphetamine [Adderall], methylphenidate [Ritalin, Concerta], lisdexamfetamine [Vyvanse]) | Agitation, hyperactivity, hypertension, mydriasis (dilation of the pupil), overheating, pacing, seizures, tachycardia, tremors |
| Antidepressants (fluoxetine [Prozac], sertraline [Zoloft], venlafaxine [Effexor]) | Agitation, diarrhea, hyperactivity, hypertension, rapid heartbeat, seizures, tremors, vomiting |
| NSAIDs (ibuprofen [Advil], naproxen [Aleve, Naprosyn], diclofenac [Voltaren]) | Abdominal pain, black or tarry stools, diarrhea, frequent urination, increased thirst, lethargy, loss of appetite, seizures, vomiting |
| Opioids (hydrocodone/acetaminophen [Norco], oxycodone [Oxycontin], fentanyl transdermal patch [Duragesic], buprenorphine [Suboxone]) | Collapse, coma, lethargy, low body temperature, pinpoint pupils, sedation, slowed breathing, unresponsiveness |
| Recreational drugs (Cannabis, cocaine, methamphetamine [Desoxyn]) | Dilated pupils, disorientation, high body temperature, hyperactivity, lethargy, seizures, stumbling, tremors, vomiting |
| ABBREVIATIONS: CNS = central nervous system | |
SIDEBAR: Universal Early Symptoms Across Agents
- Behavioral changes – restlessness, vocalization, agitation
- Cardiovascular distress – irregular heartbeat, high blood pressure, collapse
- Gastrointestinal symptoms – vomiting, excessive drooling, diarrhea
- Hyperthermia – elevated body temperature, excessive panting, drooling
- Neurological signs – tremors, disorientation, seizures, agitation
- Respiratory changes – labored breathing, excessive panting, wheezing
ADHD Medications
ADHD medications are potent central nervous system (CNS) stimulants. They have a narrow margin of safety in animals and can result in life-threatening cardiovascular or neurologic complications. Fast referral is critical. The symptoms described in Table 1 may appear within two hours.11
Antidepressants
Many antidepressants increase serotonin in humans and animals, which can cause serotonin syndrome in both species. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are common in homes and highly dangerous to pets.
NSAIDs
As noted above, pets metabolize NSAIDs designed for humans poorly, if at all. Cats and dogs tolerate diclofenac, ibuprofen, and naproxen poorly. These medications can cause ulcers, renal injury, or liver failure at human therapeutic doses. One important sign of toxicity is blood in vomit.6 Some pet owners may assume human and pet NSAIDs are interchangeable. It's important to note cats and dogs have their own species-approved NSAIDs and analgesics formulated for safer metabolism. Use of human medications without veterinary guidance can lead to serious harm.
Carprofen (Rimadyl) is a Food and Drug Administration (FDA) approved in dogs for osteoarthritis and soft tissue pain. It is highly protein‑bound and eliminated via hepatic metabolism, with metabolites excreted in feces and urine. Meloxicam (Metacam) is approved for use in dogs in the U.S., and in some regions for cats in single‑dose or limited regimens. In cats, it undergoes oxidative metabolism (rather than glucuronidation) with approximately 80% of the drug eliminated in feces. Robenacoxib (Onsior) is another NSAID used in cats and dogs (for short durations), with cautious use in cats due to their limited ability to detoxify NSAIDs. These formulations are engineered to match each species’ pharmacokinetics, metabolism, and safety thresholds, making them safer than human NSAIDs.16
Opioids
Topical patches pose a particular risk if chewed or licked. Naloxone access in veterinary settings has become increasingly important. A 2020 study looked at 189,594 calls to the ASPCA’s APCC involving opioids from 2006 to 2014.14 It found small, young, intact (compared to neutered) dogs living in areas with high opioid prescribing were more likely to be involved in opioid-related emergency calls. Smaller and younger dogs were at higher risk than larger and older dogs. These researchers also found veterinarians were more likely to call the poison control hotline than owners. Owners may be reluctant to report exposures to illicit opioids. The research showed a strong positive non-linear link between dog poisonings and local opioid prescription rates.14
Recreational Drugs (Marijuana, Cocaine, Methamphetamine, Psilocybin)
Tetrahydrocannabinol (THC) and stimulants affect pets differently than humans, often with prolonged or unpredictable effects. Marijuana, cocaine, and methamphetamine can cause severe toxicity.15 Pets may appear frightened or "zoned out."
As marijuana becomes legal in more states, accidental pet exposures are rising—and costly. Pet health insurance provider Trupanion reported 1,852 marijuana-related toxicity claims over five years, mostly from pets ingesting edibles, plants, or baked goods. Figure 1 shows poisoning rates are higher in states with legalized recreational marijuana. Since 2020, California led with 428 claims, followed by Massachusetts, New York, and Florida.17

Figure 1. Marijuana Toxicity-Related Claims in Dogs & Cats in 202417
Pharmacists and technicians should treat any known ingestion of these medications by a pet as an urgent referral to ASPCA APCC or Pet Poison Helpline. Ideal documentation would include the brand, strength, dosage form, and time of ingestion. Pharmacy staff should encourage owners to have the information handy when calling and to take the packaging with them to the veterinarian. Even if the owner reports their pet “seems fine” hours after exposure, toxicity can be delayed or progressive and serious harm may still occur without visible symptoms. Erring on the side of caution and referring patients and their pets to a veterinarian immediately is crucial.
Other Common Toxins
Human formulations may contain excipients or flavoring agents that are hazardous to pets. Certain gabapentin oral solutions contain xylitol (also labeled as birch sugar), which is rapidly toxic to dogs in small amounts. Xylitol triggers a potent insulin release in dogs, leading to hypoglycemia within 15 to 30 minutes. Symptoms often begin with vomiting and progress to lethargy, ataxia, tremors, seizures, or collapse. In severe cases or with higher doses, liver failure can occur.18 Pharmacists must check for inactive ingredients in liquid formulations and educate pet owners about this. It is important to note that xylitol is found in many common household items, including peanut butter and sugar-free candy.
Dogs are commonly prescribed levothyroxine to treat hypothyroidism and typically require significantly higher doses per kilogram of body weight than humans. Dosing must be carefully titrated, with regular monitoring of serum T₄ levels to avoid under- or over-dosing. Cats experience hyperthyroidism more often, and are treated with methimazole or radioactive iodine. They rarely need levothyroxine unless iatrogenic hypothyroidism occurs. Differences in thyroid disorders, metabolism, and treatment protocols make it dangerous to assume human thyroid medication doses apply to pets.19
Prednisone dosages vary based on whether the animal is being treated for inflammation or for immune suppression, as higher doses are typically required for immunosuppressive effects. Cats metabolize corticosteroids differently than dogs and humans, requiring different dosing protocols and careful consideration of duration and tapering. In dogs, veterinarians commonly use prednisone to manage allergic, musculoskeletal, or autoimmune conditions. Prolonged use requires monitoring for adverse effects such as polyuria (frequent urination), polydipsia (unusual thirst), or gastrointestinal ulceration.20 In cats, prescribers often prefer prednisolone (rather than prednisone) because of their reduced hepatic conversion capacity, making direct administration of the active form more effective and safer.21
Even a single tablet of acetaminophen may be enough to kill a cat. In one published case, a cat experienced acetaminophen toxicity after exposure to a single dose. The patient exhibited hallmark signs such as cyanosis and facial swelling. The case highlighted the need for rapid intervention, and the diagnostic challenge this toxicosis can present. This report highlights the narrow safety margin of acetaminophen in cats and the importance of pharmacist awareness when reviewing shared medications between humans and pets.22
PAUSE AND PONDER: If a pet owner says, “My dog is acting weird today after I dropped my pill,” what specific behaviors or symptoms should prompt you to refer them to a veterinarian or poison control center?
CLINICAL SIGNS OF TOXICITY IN PETS
A common question a pharmacy professional might hear from a pet owner is, "How do I know if my pet is poisoned?" Often, symptoms go unnoticed until they’re severe, and by then, the window for successful treatment may have narrowed. Pharmacists and technicians can recognize red flags early.
This section outlines key clinical signs of toxicity in pets across various drug classes, with an emphasis on phrases owners might use when describing the issue. This helps pharmacy teams know when to probe further and when to refer to a veterinarian or animal poison control center.
Tails of Toxicity
Pets may exhibit nonspecific signs that warrant urgent attention. Since pets cannot verbalize how they are feeling, owners must rely on observation of behavioral changes or physical symptoms. Table 2 lists ways to determine if a pet is ill.
Table 2. Analyzing Pet Behaviors for Signs of Poisoning4, 23-25
| Clinical Manifestation | Points to Remember |
| Lethargy or weakness | The owner may say “She’s not acting like herself,” or “He’s been sleeping all day.” |
| Vomiting and/or diarrhea | Immediate referral is warranted, especially if it is persistent, contains blood, or is paired with other symptoms. |
| Loss of appetite | The owner may report the pet eating only part of the regular meal size, skipping meals, or refusing favorite treats. |
| Tremors or seizures | ● Often, owners see twitching, drooling, or frothing at the mouth and don’t realize the pet is experiencing a seizure. This often appears with exposure to stimulants (e.g., ADHD medications, pseudoephedrine, caffeine).
● Pet owners should stay calm, move nearby objects so the pets cannot knock them over or harm themselves. They should not touch or restrain the animal. They should also time how long the seizure lasts. |
| Hyperthermia | ● Cats and dogs have a narrow normal temperature range (approximately 100-102.5°F).
● A body temperature of above 102.5-103°F in cats and dogs is considered hyperthermic and can lead to tissue damage or organ stress. ● Having a rectal or digital thermometer at home is important because pets don’t display fever the way humans do. The only reliable way to detect a fever in cats and dogs is by taking their rectal temperature. |
| Ataxia (uncoordinated movement) | The owner might say “He’s stumbling all over the place.” |
| Collapse or unconsciousness | ● This is an emergency situation—immediate referral is critical.
● Advise owners to call ahead and tell the veterinary service they are on the way. If the pet is large, advise them to get help, and place the animal on a hard flat surface (i.e., an ironing board or a piece of plywood). |
| Changes in urination | This includes increased frequency (polyuria) or total suppression (anuria, especially with NSAID or antidepressant toxicity). |
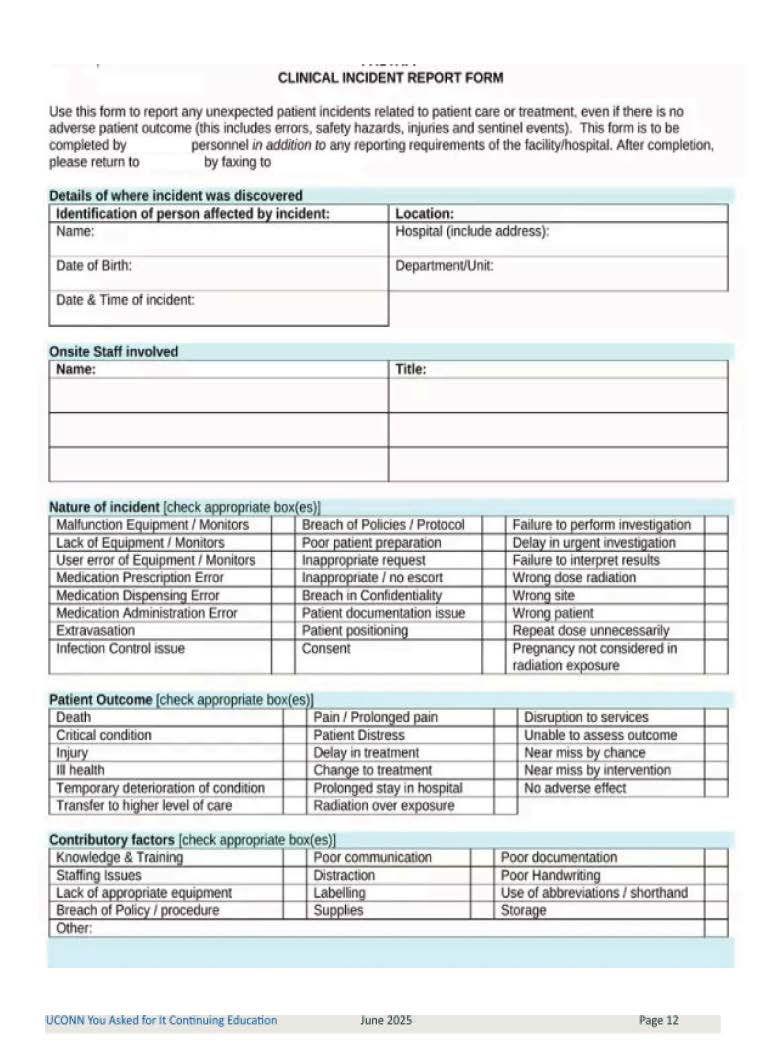
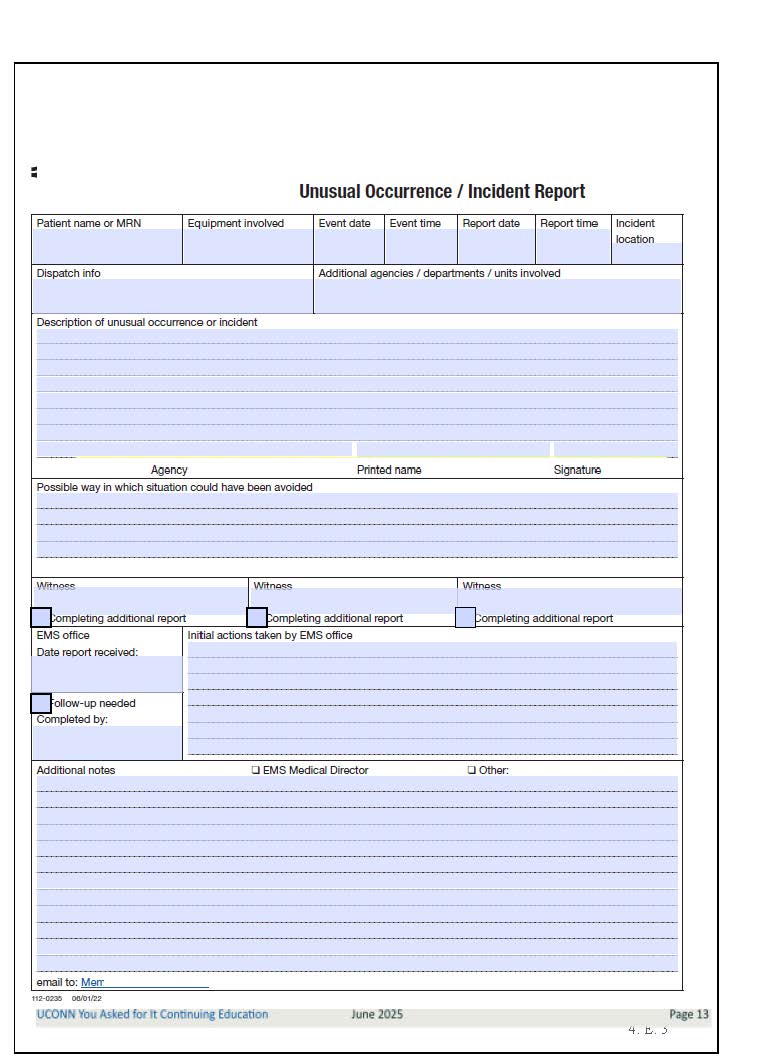
VETERINARY RESPONSE: MANAGEMENT & TREATMENT
Veterinary intervention is critical in pet poisoning cases. Most toxic exposures require decontamination, symptomatic management, and monitoring.7
Assessment and Diagnosis
Veterinarians rely heavily on the owner’s report. The most helpful information a pharmacy professional can encourage owners to bring to the vet includes 26
- The exact name of the medication ingested
- Strength and dosage form (e.g., extended-release, chewable, liquid)
- Approximate time of ingestion
- Estimated number of pills or quantity consumed
- The observed symptoms
- The pet’s weight and species
Veterinarians perform a thorough clinical examination, medical history, and toxicology screening. They will assess the pet’s vital signs (heart rate, respiratory rate, temperature) and observe neurologic status (agitation, tremors, seizures). They will also determine if the pet is suffering with dehydration or shock, and start supportive care based on the suspected toxin and symptoms.
Common diagnostic tests used in suspected poisoning cases include bloodwork and biochemical panels to assess organ function, glucose levels, and electrolyte imbalances. Urinalysis is often performed to detect drug metabolites and evaluate kidney function. Imaging techniques, such as X-rays and ultrasound, help identify ingested pills. Electrocardiography is used to monitor for cardiac abnormalities.7
Decontamination Strategies
Removing toxins from the body prevents further absorption. Veterinarians use multiple decontamination methods based on the substance and time since ingestion. Induced emesis (causing the animal to vomit) is often used within two hours of exposure. Apomorphine (in dogs) or xylazine/medetomidine (in cats) are commonly used to induce vomiting when appropriate. Hydrogen peroxide may be used in dogs, but its use is declining due to the risk of esophagitis and gastroenteritis even at therapeutic doses.25 Highly acidic or alkaline chemicals can burn the mouth and digestive tract wall if regurgitated. The veterinarian may administer activated charcoal to absorb toxins and limit further drug absorption in the gastrointestinal tract. In more severe cases, gastric lavage (stomach pumping) is performed under anesthesia, particularly for life-threatening poisonings involving opioids or stimulants.25
PRO TIP: Pharmacy teams can emphasize that inducing vomiting at home using hydrogen peroxide or other DIY methods can be dangerous. Owners shouldn’t attempt it without veterinary instruction.
Symptom Management
Veterinary treatment focuses on stabilization and organ protection. Table 3 describes specific therapies depending on the drug involved and clinical symptoms. Outcomes depend on the timing of intervention, known or suspected dosage, and pet health status. Delayed treatment increases risks of organ damage, seizures, or fatal outcomes. Follow-up veterinary care ensures no lingering effects on liver, kidneys, or heart function.
Table 3. Pet Toxicity Treatments15,27
| Toxicity Type | Treatment | Purpose |
| Cardiovascular | Beta-blockers (propranolol, atenolol) | Stabilizes heart rate and blood pressure |
| IV lipid emulsion therapy | Reduces systemic circulation of lipophilic drugs like THC and certain antidepressants | |
| Oxygen therapy and mechanical ventilation | Used in opioid-induced respiratory depression | |
| Gastrointestinal | Gastroprotectants (sucralfate, omeprazole, misoprostol) | Prevent stomach ulcers caused by NSAIDs. |
| Liver protectants (SAMe, silymarin) | Supports liver function in cases of acetaminophen or NSAID toxicity | |
| Neurological | Cooling measures | Used in hyperthermic pets with stimulant toxicity |
| Sedation (benzodiazepines, barbiturates) | Controls seizures and agitation | |
| IV fluid therapy | Prevents dehydration and supports kidney function | |
| ABBREVIATIONS: IV = intravenous; NSAID = nonsteroidal anti-inflammatory drug; THC = tetrahydrocannabinol | ||
Antidotes and Specialized Therapies
In some poisonings, antidotes are available. Table 4 lists specific reversal agents.
Table 4. Toxins and Their Antidotes7
| Toxin | Antidote | |
| Acetaminophen | N-acetylcysteine | |
| Alpha-2 agonists | Atipamezole (in some cases) | |
| Benzodiazepines | Flumazenil | |
| Opioids | Naloxone |
Use of naloxone deserves extra attention. If a pet consumes an opioid and has collapsed, lost consciousness and/or has shallow breathing, owners can administer naloxone intranasally. Ideally, owners should administer naloxone under the direction of a veterinarian, who would determine the dose. Canine police officers have naloxone on hand because they have a prescription and are given detailed instructions on how to administer it. Regardless of who administers the naloxone, pets need to be taken to emergency care immediately after receiving the dose. Owners who have opioids in the home for prescribed or recreational use should be trained to use naloxone before an emergency happens.28
Exposures to many medications, like antidepressants or ADHD medications, have no direct antidote. Management focuses on controlling symptoms and preventing complications. While many pets make full recoveries, outcomes depend on the type and amount of drug ingested, the time between ingestion and treatment, the pet’s size and species, and access to antidotes or critical care. Some cases (e.g., extended-release ADHD medications in small dogs) can be fatal even with treatment.
Costs and Outcomes
Veterinary care for toxicity can be expensive. Some ER visit costs include29
- ER exam: ~ $100 – $200
- IV catheter: ~ $60 – $75
- IV fluids (per bag): ~ $60 – $95
- Blood tests (basic): ~$80 – $200
- Urine tests (basic): ~$40 – $70
- X-ray (basic): ~$150 – $250
- Ultrasound: ~ $300 – $600
- Blood pressure measurement: ~ $25 – $75
- Pain medication: ~ $40 – $80
- Oxygen therapy: ~ $500 – $3,000
- Wound treatment and repair: ~ $800 – $2,500
- Emergency surgery (bloat, foreign body, hit by care, caesarian): ~ $1,500 – $5,000
- Hospitalization and monitoring:
- 1 – 2 days (vomiting, diarrhea, seizures cases): ~ $600 – 1,700
- 3 – 5 days (parvo, blocked cat, kidney failure): ~ $1,500 – $3,500
The Pharmacy Team’s Duty
When a poisoning occurs or is suspected, pharmacy employees can help in three ways. They can provide medication bottle labels or manufacturer information for veterinarians, reinforce that owners shouldn’t wait for symptoms to appear, and help set expectations about potential costs. A better way to deal with this issue is to implement preventive measures.
PREVENTION: PAWS OFF THE PILLS
Veterinary professionals stress education, secure medication storage, and responsible disposal practices to reduce the chances of pet poisonings. Pet owners are responsible for ensuring a safe environment free from toxic drug exposure.
Keeping drugs out of reach helps prevent accidental ingestion. Veterinary toxicologists recommend using childproof containers, since pets can easily chew through standard plastic pill bottles. Pet owners should store medications in cabinets with secure latches, as pets—especially cats—can access countertops and nightstands.30 It is important to keep bags closed, because pets can get into backpacks or handbags containing loose medications.
Improper disposal of medications increases the risk of pet exposure. Veterinary professionals advise using take-back programs, as many pharmacies and veterinary clinics offer safe disposal services for unused medications. Discarded medications should be sealed in containers, such as plastic bags filled with coffee grounds or cat litter, to discourage pets from scavenging through trash bins. In some cases, the FDA recommends flushing high-risk drugs, such as opioids, to prevent exposure to humans and pets. These drugs are on the FDA's "Flush List" due to their danger if used by anyone other than the prescribed individual. Flushing these medications is only advised when a take-back option is not readily available.30
COUNSELING POINTS FOR PET-OWNING PATIENTS
Pharmacists and pharmacy technicians are well-positioned to help prevent pet poisonings by proactively counseling pet-owning patients. These conversations don’t need to be long—but they need to be specific, timely, and relevant to the patient’s situation. The goal is to raise awareness, encourage safe practices, and direct patients to resources before an emergency occurs.31
Proactive counseling doesn’t just protect pets. It builds trust with patients, strengthens the pharmacist’s contribution in the community, and positions the pharmacy as a reliable source for pet-related safety guidance.31
Sniffing Out Red Flags
Counseling opportunities often arise when patients pick up medications known to be toxic to pets (e.g., antidepressants, ADHD medications, liquid gabapentin, NSAIDs, opioids). Patients may mention they have a new pet or ask about pet-related topics. Pharmacy staff may also notice a customer has pet-related OTC products in their basket (e.g., flea treatments, joint supplements, pet toothpaste). Sometimes, pets appear in the background of a telepharmacy call or accompany the owner into the store. All of these situations may prompt a discussion about medication toxicity.
Tips for Technicians
Technicians are often the first team member a patient interacts with. They can 31
- Ask, "Do you have pets at home?" when checking out medications
- Flag high-risk medications that are toxic to pets
- Share printed materials or magnets with animal poison control info
- Update standard operating procedures to include referral language for veterinary poison concerns
- Give a reminder at the register when a patient picks up a flavored ADHD medication
- Refer to the pharmacist any time a pet is mentioned in relation to medications
Fetch the Right Tools
- Keep a laminated cheat sheet behind the counter with common pet-toxic medications
- Use stickers on vials to warn of danger to pets (e.g., "TOXIC TO PETS – KEEP OUT OF REACH")
- Partner with local veterinary clinics to distribute safety flyers
PAUSE AND PONDER: What would you say to a pet owner who asks you to help them “put their dog down” because they can’t afford treatment after a drug exposure incident?
PETS AND PENALTIES
Accidental drug exposure in pets presents legal and ethical concerns. Pet owners must ensure their pet’s safety, while veterinarians navigate ethical obligations when treating drug-related poisonings.32
Laws regarding pet poisoning vary by state, but owners can face legal consequences if their negligence results in harm. Unintentionally or intentionally exposing pets to drugs may lead to negligence claims, with owners remaining civilly liable for preventable injuries. In some states, reckless or intentional poisoning is classified as animal cruelty and can result in misdemeanor or felony charges.32 Recreational drug-related poisonings, especially those involving THC, have also brought increased legal scrutiny to pet owners in states where cannabis is legal.12
In several states, veterinary professionals are classified as mandatory reporters of suspected neglect or abuse. In cases of drug toxicity, ethical dilemmas often arise. Veterinarians must weigh client confidentiality against their duty to report suspected drug-related neglect. Some pet owners request euthanasia instead of pursuing costly treatment, raising additional ethical concerns. Legal protections for veterinarians who report drug-related neglect, such as immunity laws, are continuing to evolve.32
Understanding the Pharmacy Boundaries
Pet poisoning incidents that stem from human medication exposure often raise legal and ethical questions for pharmacy professionals. Pharmacists and pharmacy technicians must understand their scope of practice and operate within it, while still providing meaningful support to pet-owning patients.33
Pharmacists are legally bound to avoid giving direct medical advice about animal-specific treatment unless they are licensed veterinarians or have specialized training in veterinary pharmacy. Examples that are out of the pharmacist’s scope of practice include suggesting a dosage of activated charcoal or recommending OTC human medications for a pet without a veterinarian’s guidance. Doing so may open the door to legal liability, even if intentions are good.33 Pharmacists should document counseling as they do with any human consultation when possible. The pet owner is ultimately responsible for storing their medications safely. However, pharmacy staff may bear ethical responsibility if they miss clear opportunities to prevent harm. For example, pharmacy staff must check that the medication strength and instructions align with veterinary guidance. It's a pharmacist’s duty to promote medication safety.31
With the rise in pet prescriptions being filled at human pharmacies, another legal concern has emerged. Medications like amoxicillin, gabapentin, prednisone, and levothyroxine are commonly prescribed to both humans and animals. However, the dosages, formulations, and routes of administration can differ. It is unsafe to give dogs human‑formulated gabapentin liquid—these often contain xylitol. Gabapentin for pets should only be used under veterinary supervision with a weight‑based dose.34 Pharmacists must exercise due diligence in checking drug references that include veterinary considerations, such as VetMedux and Plumb’s Veterinary Pharmacy, especially when unfamiliar with a prescription’s purpose.
While legal boundaries are clear, ethical considerations require pharmacy staff to act with compassion, respect, and clarity. Pet owners in crisis may arrive at the counter distraught, panicked, or angry. Some may be grieving a pet’s death. If that happens, pharmacy staff must acknowledge the emotional distress and not minimize or dismiss the concerns. They can say, “We’re not veterinarians, but here’s what I can do to help.” The staff should refer owners clearly and quickly, providing poison control numbers, emergency vet locations, or printouts.
In cases where a pet owner requests euthanasia due to financial constraints after a drug exposure, veterinary and pharmacy professionals must respond with empathy but remain ethically grounded. A compassionate response might be: “I’m sorry you’re going through this. While I can’t give treatment advice, I urge you to contact an emergency veterinarian—there may be lower-cost options or payment plans available.” This approach balances empathy, defers clinical decisions to appropriate professionals, and reinforces that a pet’s life may still be saved with timely care.
A PET-SAFE FUTURE
In the evolving landscape of pharmacy practice and public health, one area rapidly gaining attention is the intersection of human medications and companion animal safety. The COVID-19 pandemic increased pet adoption rates and work-from-home opportunities. The overall shift in household routines has created new opportunities—and new risks—for pet exposures to toxic substances.
Ongoing research continues to improve diagnostic tools and treatment options for pets exposed to human medications. Future innovations include the development of rapid toxicology screening kits that allow faster, in-clinic detection of opioids, amphetamines, and antidepressants. Additionally, genetic studies on drug metabolism aim to identify species-specific sensitivities, helping to advance more personalized approaches in veterinary care.8
Many states now require cannabis products to be sold in child-resistant, often opaque, packaging to reduce the risk of accidental ingestion, particularly in children.35 These measures may also help limit accidental exposures in pets. As telehealth and online pharmacy services expand, fewer patients are interacting face-to-face with pharmacists.36 This limits opportunities to reinforce safe medication storage. As a result, it becomes essential for pharmacists and technicians to include safety messaging on prescription labels, auxiliary stickers, or digital communications.
Digital Defenses
Advances in technology are improving awareness, prevention, and emergency response for pet poisoning cases. Future tools include AI-powered toxicology apps that provide instant poisoning risk assessments and smart storage systems like electronic pill dispensers to prevent accidental exposures.37,38 Wearable pet monitors may also detect toxicity through changes in heart rate or body temperature.39 These innovations aim to support pet owners and veterinarians in managing drug-related emergencies more effectively.
Other tools are being developed to assist in identifying potential poison risks. These include the ASPCA APCC app, offering a searchable database of common toxins, and ASPCA AnTox database—a veterinary database system to help identify and characterize toxic exposure data. In the future, pharmacy software may integrate pet-safety alerts when filling medications known to be high risk. Until then, it falls on pharmacy professionals to stay educated and vigilant.
CONCLUSION
The rising incidence of pet poisonings due to human medications is more than an unfortunate trend—it’s a public health concern extending beyond species lines. Pharmacy professionals are often the first point of contact for patients navigating their own medications and their households’ safety practices. Future research will continue improving diagnosis, treatment, and toxicology education. Collaboration between veterinarians, policymakers, and pet owners remains essential to reducing risks. Let’s increase awareness and protect all members of the household—on two legs and four.
Pharmacist Post Test (for viewing only)
PATIENT SAFETY: Toxic Human Drugs and Their Impact on Household Pets
26-001 Pharmacist Post-test
After completing this continuing education activity, pharmacists will be able to:
● DESCRIBE common pathways through which pets are exposed to toxic human medications
● IDENTIFY the clinical signs and symptoms of toxicity from antidepressants, ADHD medications, NSAIDs, opioids, and recreational drugs in companion animals
● DISCUSS veterinary management strategies and outcomes for pets exposed to toxic medications, including decontamination, symptom management, and diagnostic testing
● RECOGNIZE best practices to counsel pet-owning patients on safe medication storage, disposal, and early signs of pet poisoning
*
1. Which of the following statements is TRUE regarding pet exposure to human medications?
A. Cats and dogs have the same liver enzymes as humans and can metabolize medications similarly
B. Human medications now account for fewer poisonings in pets than chocolate or household cleaners
C. Even small doses of human medications can be toxic to pets due to species-specific metabolism
*
2. A 35 lb Labrador retriever is brought to the veterinary clinic one hour after chewing through and ingesting an unknown quantity of its owner’s fluoxetine (Prozac). Which of the following symptoms is most likely to be observed?
A. Bradycardia, lethargy, and coma
B. Vomiting, tremors, and hyperactivity
C. Constipation, slow breathing, and pinpoint pupils
*
3. Which of the following best describes secondary exposure in the context of pet poisoning?
A. A pet inhaling prescription aerosol medications left on a counter
B. A pet licking topical medication off a human’s skin
C. A pet chewing through an unopened blister pack of pills
*
4. A dog is brought to the veterinary clinic after ingesting an unknown medication from the street. A few hours later, the dog begins vomiting and shows signs of lethargy. Bloodwork reveals early signs of kidney impairment. Which class of medication is most likely responsible for these symptoms?
A. SSRIs
B. Amphetamines
C. NSAIDs
*
5. Which of the following is part of standard veterinary decontamination for a recent ingestion of a toxic medication?
A. Naloxone and activated charcoal only
B. Induced vomiting, activated charcoal, and supportive care
C. Benzodiazepines and antipsychotics
*
6. A man brings a dog into the emergency veterinary clinic late at night. The owner admits that an edible marijuana product may have gone missing from the kitchen counter. The dog is showing abnormal behavior. The veterinary team suspects a toxic ingestion. Which of the following combinations of symptoms would best support the suspected diagnosis?
A. Agitation, seizures, and vomiting
B. Excessive drooling, tremors, and elevated body temperature
C. Stumbling, lethargy, and dilated pupils
*
7. Which of the following is a correct counseling point for a patient asking how to dispose of unused opioids in a pet-safe manner, assuming a take-back program is unavailable?
A. Flush the medication only if it’s on the FDA flush list
B. Mix the medication with cat litter and throw it in an open trash bin
C. Store it on the kitchen counter until you need it again
*
8. What is a legal or ethical concern pharmacists should be aware of when advising pet owners about medication safety?
A. Veterinarians are never required to report suspected neglect involving pet poisonings
B. Euthanasia is always recommended in cases of drug ingestion due to cost
C. Pet owners can face civil or criminal liability for preventable poisonings
*
9. A patient mentions her dog chewed up her partner’s Adderall, but “seems fine now.” What is the BEST pharmacist response?
A. “Monitor the dog at home and call a veterinarian only if symptoms start.”
B. “Give the dog a dose of diphenhydramine to counteract the stimulant.”
C. “Take the dog to a veterinarian or emergency clinic immediately.”
*
10. A pet owner asks whether topical lidocaine cream could harm his cat, who licked some off her hand. What is the most appropriate next step?
A. Reassure them that lidocaine is safe for cats in small doses
B. Tell them to wash the cat’s mouth with water and monitor at home
C. Advise them to call a veterinary-specific poison control center
Pharmacy Technician Post Test (for viewing only)
PATIENT SAFETY: Toxic Human Drugs and Their Impact on Household Pets
26-001 Technician Post-test
After completing this continuing education activity, pharmacy technicians will be able to:
● RECOGNIZE common human medications that are toxic to pets
● IDENTIFY signs and symptoms of drug toxicity in companion animals that may be mentioned by pet owners at the pharmacy counter
● LIST proper techniques for medication storage and disposal that can reduce the risk of pet exposure
● RECOGNIZE when to refer pet-owning patients to the pharmacist for counseling or poison control center guidance
*
1. What is the BEST way to store prescription medications to prevent pet exposure?
A. On a high shelf in the kitchen next to food storage
B. In a closed cabinet or drawer out of reach of pets
C. On a bedside table for easy access
*
2. A pharmacist receives a phone call from a pet owner who is panicked because her dog is stumbling and uncoordinated. Which of the following substances is the most likely cause of the dog’s symptoms?
A. Adderall
B. Aspirin
C. Cannabis
*
3. What is the most important action a technician should take when a pet owner mentions their animal ingested human medication?
A. Suggest giving the pet activated charcoal from the pharmacy
B. Tell them to watch for symptoms before doing anything
C. Refer them to the pharmacist or a poison control center
*
4. A pharmacy technician receives a call from a pet owner who says his dog chewed through a pill bottle that had fallen on the floor. The label reads “Adderall XR 20 mg.” Which of the following symptom combinations best aligns with amphetamine toxicity in pets?
A. Lethargy, cold paws, and vomiting
B. Hyperactivity, tremors, and increased heart rate
C. Head tilt, circling, and loss of balance
*
5. Which medication class is known to cause ulcers and kidney damage in pets?
A. SSRIs
B. NSAIDs
C. Benzodiazepines
*
6. A cat owner calls their local pharmacy and asks whether their pet can take the same OTC pain medication they use. What should the pharmacist do?
A. Recommend a small dose based on the cat’s weight
B. Advise the owner to contact their veterinarian before giving any medication
C. Suggest a liquid version of the same drug for easier swallowing
*
7. An owner rushes her pet to the clinic after it chewed through a prescription bottle labeled "fluoxetine." Which symptoms will likely occur?
A. Seizures, vomiting, and slowed breathing
B. Vomiting, tremors, and hyperactivity
C. Dehydration and joint pain
*
8. A patient picks up a prescription for a topical hormone patch. What should a technician do if the patient mentions having a cat?
A. Say nothing; the pharmacist will handle it later
B. Tell them the patch is safe as long as the cat doesn’t lick it
C. Refer the patient to the pharmacist to explain the risk of secondary exposure
*
9. Which of the following is a proper disposal method for unused opioids that prevents pet access?
A. Throw the bottle in the trash
B. Use a take-back program or follow FDA flush list
C. Leave them on a shelf for future use
*
10. A customer picks up his prednisone prescription and mentions that he’s been giving a “small amount” of his prednisone to his dog because the dog seems itchy. He asks if it’s okay to continue. As the pharmacy technician, what is the best action?
A. Tell the customer that prednisone is commonly used in dogs and they can continue for a few days
B. Suggest the customer purchase an over-the-counter antihistamine formulated for pets instead C. Say you cannot provide advice for animals and refer the question to the pharmacist, who may contact animal poison control if needed
C. Say you cannot provide advice for animals and refer the question to the pharmacist, who may contact animal poison control if needed
References
Full List of References
1. The Official Top 10 Toxins of 2024. ASPCA. March 13, 2025. Accessed October 2, 2025. https://www.aspca.org/news/official-top-10-toxins-2024
2. Cortinovis C, Pizzo F, Caloni F. Poisoning of dogs and cats by drugs intended for human use. Vet J. 2015;203(1):52-58. doi:10.1016/j.tvjl.2014.11.004
3. 70% of U.S. households have pets, APPA finds in new survey. Veterinary Advantage. June 2021. Accessed September 20, 2025. https://vet-advantage.com/companion-news/70-of-u-s-households-have-pets-appa-finds-in-new-survey/
4. Fitzgerald KT, Bronstein AC, Flood AA. "Over-the-counter" drug toxicities in companion animals. Clin Tech Small Anim Pract. 2006;21(4):215-226. doi:10.1053/j.ctsap.2006.10.006
5. Sjöström K, Mount J, Klocker AK, Arthurson V. A review of adverse events in animals and children after secondary exposure to transdermal hormone-containing medicinal products. Vet Rec Open. 2022;9(1):e48. Published 2022 Oct 28. doi:10.1002/vro2.48
6. Khan SA, McLean MK. Toxicology of frequently encountered nonsteroidal anti-inflammatory drugs in dogs and cats. Vet Clin North Am Small Anim Pract. 2012;42(2):289-vii. doi:10.1016/j.cvsm.2012.01.003
7. Houchen E. Recognizing & treating toxicities. Oregon Veterinary Medical Association. Accessed September 10, 2025. https://www.oregonvma.org/sites/default/files/Houchen%20Recognizing%20%26%20Treating%20Toxicities.pdf
8. Court MH. Feline drug metabolism and disposition: pharmacokinetic evidence for species differences and molecular mechanisms. Vet Clin North Am Small Anim Pract. 2013;43(5):1039-1054. doi:10.1016/j.cvsm.2013.05.002
9. Lees P, Pelligand L, Elliott J, Toutain PL, Michels G, Stegemann M. Pharmacokinetics, pharmacodynamics, toxicology and therapeutics of mavacoxib in the dog: a review. J Vet Pharmacol Ther. 2015;38(1):1‑14. doi:10.1111/jvp.12185.
10. Pet Poison Helpline: 24/7 animal poison control center. Pet Poison Helpline. Accessed September 19, 2025. https://www.petpoisonhelpline.com/
11. Stern L, Schell M. Management of Attention-Deficit Disorder and Attention-Deficit/Hyperactivity Disorder Drug Intoxication in Dogs and Cats: An Update. Vet Clin North Am Small Anim Pract. 2018;48(6):959-968. doi:10.1016/j.cvsm.2018.07.007
12. Fitzgerald KT, Bronstein AC, Newquist KL. Marijuana poisoning. Top Companion Anim Med. 2013;28(1):8-12. doi:10.1053/j.tcam.2013.03.004
13. Pugh CM, Sweeney JT, Bloch CP, Lee JA, Johnson JA, Hovda LR. Selective serotonin reuptake inhibitor (SSRI) toxicosis in cats: 33 cases (2004-2010). J Vet Emerg Crit Care (San Antonio). 2013;23(5):565-570. doi:10.1111/vec.12091
14. Howard-Azzeh M, Pearl DL, O'Sullivan TL, Berke O. The identification of risk factors contributing to accidental opioid poisonings in companion dogs using data from a North American poison control center (2006-2014). PLoS One. 2020;15(1):e0227701. doi:10.1371/journal.pone.0227701
15. Oster E, Čudina N, Pavasović H, et al. Intoxication of dogs and cats with common stimulating, hallucinogenic and dissociative recreational drugs. Vet Anim Sci. 2023;19:100288. Published 2023 Jan 31. doi:10.1016/j.vas.2023.100288
16. Edwards SG. Nonsteroidal Anti-Inflammatory Drugs in Animals. Merck Veterinary Manual. Updated September 2024. Accessed October 17, 2025. https://www.merckvetmanual.com/pharmacology/inflammation/nonsteroidal-anti-inflammatory-drugs-in-animals
17. California tops list of marijuana toxicity cases in pets, new data shows. Veterinary Practice News. April 21, 2025. Accessed April 22, 2025. https://www.veterinarypracticenews.com/marijuana-toxicity-pets/
18. Hayes C. Xylitol Toxicosis in Dogs. Merck Veterinary Manual. Revised September 2024, modified June 2025. Accessed October 21, 2025. https://www.merckvetmanual.com/toxicology/food-hazards/xylitol-toxicosis-in-dogs
19. Heseltine J, Kritchevsky J. Hypothyroidism in Animals. Merck Veterinary Manual. Revised May 2024, modified May 2025. Accessed October 21, 2025. https://www.merckvetmanual.com/endocrine-system/the-thyroid-gland/hypothyroidism-in-animals
20. Edwards SH. Corticosteroids in Animals. Merck Veterinary Manual. Revised November 2021, modified May 2025. Accessed October 21, 2025. https://www.merckvetmanual.com/pharmacology/inflammation/corticosteroids-in-animals
21. Forsythe LR, Gollakner R. Prednisone in Dogs & Cats: Uses & Side effects. VCA Animal Hospitals. 2024. Accessed December 2, 2025. https://vcahospitals.com/know-your-pet/prednisoloneprednisone
22. Allen AL. The diagnosis of acetaminophen toxicosis in a cat. Can Vet J. 2003;44(6):509-510. https://pmc.ncbi.nlm.nih.gov/articles/PMC340185/
23. Fever in Dogs and Cats. Schwarzman American Medical Center. Updated June 17, 2024. Accessed October 4, 2025. https://www.amcny.org/pet_health_library/does-my-pet-have-a-fever/
24. Morrison B. What Things Are Poisonous to Cats? PetMD. Updated November 11, 2025. Accessed December 2, 2025. https://www.petmd.com/cat/poisoning/poisons-in-cats
25. Lee JA. Therapeutic Updates in Veterinary Toxicology. Today’s Veterinary Practice. July/August 2014. Accessed December 2, 2025. https://todaysveterinarypractice.com/toxicology/therapeutic-updates-in-veterinary-toxicology/
26. What to expect when calling ASPCA Animal Poison Control Center. ASPCA. April 1, 2020. Accessed September 19, 2025. https://www.aspca.org/news/what-expect-when-calling-aspca-animal-poison-control-center
27. Gwaltney-Brant S, Meadows I. Use of intravenous lipid emulsions for treating certain poisoning cases in small animals. Vet Clin North Am Small Anim Pract. 2012;42(2):251-vi. doi:10.1016/j.cvsm.2011.12.001
28. Dodman DrN. Naloxone (Narcan®) for Dogs and Cats. PetPlace. July 16, 2015. Accessed October 10, 2025. https://www.petplace.com/article/drug-library/drug-library/library/naloxone-narcan-for-dogs-and-cats
29. Pet emergency statistics and veterinary costs. Preventive Vet. Accessed December 5, 2025. https://www.preventivevet.com/pet-emergency-statistics
30. Properly store medications to keep your pet safe. U.S. Food and Drug Administration. Updated June 14, 2024. Accessed April 27, 2025. https://www.fda.gov/animal-veterinary/animal-health-literacy/properly-store-medications-keep-your-pet-safe
31. Immonen H, Raekallio MR, Holmström AR. Promoting veterinary medication safety - Exploring the competencies of community pharmacy professionals in veterinary pharmacotherapy. Vet Anim Sci. 2023;21:100310. Published 2023 Aug 19. doi:10.1016/j.vas.2023.100310
32. Arkow P, Boyden P, Patterson-Kane E. Practical Guidance for the Effective Response by Veterinarians to Suspected Animal Cruelty, Abuse and Neglect. American Veterinary Medical Association; 2013. Accessed April 27, 2025. https://www.avma.org/sites/default/files/2023-12/AVMA-Suspected-Animal-Cruelty.pdf
33. Pharmacy and prescription issues. American Veterinary Medical Association. Accessed September 19, 2025. https://www.avma.org/resources-tools/animal-health-and-welfare/animal-health/pharmacy.
34. Gabapentin. VCA Animal Hospitals. Accessed October 17, 2025. https://vcahospitals.com/know-your-pet/gabapentin
35. Swinburne M. Cannabis regulation: packaging restrictions to reduce appeal to children [fact sheet]. Network for Public Health Law; October 25, 2022. Accessed April 27, 2025. https://www.networkforphl.org/wp-content/uploads/2022/11/Packaging-Regulation.pdf
36. Chong RLK, Chan ASE, Chua CMS, Lai YF. Telehealth Interventions in Pharmacy Practice: Systematic Review of Reviews and Recommendations. J Med Internet Res. 2025;27:e57129. Published 2025 May 7. doi:10.2196/57129
37. Hartung T. Artificial intelligence as the new frontier in chemical risk assessment. Front Artif Intell. 2023;6:1269932. doi:10.3389/frai.2023.1269932
38. Faisal S, Ivo J, Patel T. A review of features and characteristics of smart medication adherence products. Can Pharm J (Ott). 2021;154(5):312-323. Published 2021 Jul 30. doi:10.1177/17151635211034198
39. Riddick K. Wearable Technology in Veterinary Medicine. Georgia Veterinary Medical Association. September 18, 2024. Accessed April 27, 2025. https://gvma.net/2024/09/18/wearable-technology-in-veterinary-medicine/