Learning Objectives
After completing this application-based continuing education activity, pharmacists and pharmacy technicians will be able to:
- Review the regulatory timeline of generic drugs in the United States
- Define the regulatory and scientific criteria for therapeutic equivalence, including bioequivalence and pharmaceutical equivalence, as established by the U.S. Food and Drug Administration (FDA)
- Differentiate between brand-name, generic, and authorized generic drug products, identifying key differences in composition, cost, and approval pathways
- Discuss the clinical implications of switching between drug products, especially those with a narrow therapeutic index (NTI)
- Apply state-specific laws and the FDA's "Orange Book" and “Purple Book” to make appropriate and legally sound generic substitutions

Release Date
Release Date: December 15, 2025
Expiration Date: December 15, 2028
Course Fee
Pharmacists $7
Pharmacy Technicians $4
There is no funding for this CE.
ACPE UANs
Pharmacist: 0009-0000-25-074-H03-P
Pharmacy Technician: 0009-0000-25-074-H03-T
Session Codes
Pharmacist: 25YC74-GPW21
Pharmacy Technician: 25YC74-WGP12
Accreditation Hours
2.0 hours of CE
Accreditation Statements
| The University of Connecticut School of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Statements of credit for the online activity ACPE UAN 0009-0000-25-074-H03-P/T will be awarded when the post test and evaluation have been completed and passed with a 70% or better. Your CE credits will be uploaded to your CPE monitor profile within 2 weeks of completion of the program. |  |
Disclosure of Discussions of Off-label and Investigational Drug Use
The material presented here does not necessarily reflect the views of The University of Connecticut School of Pharmacy or its co-sponsor affiliates. These materials may discuss uses and dosages for therapeutic products, processes, procedures and inferred diagnoses that have not been approved by the United States Food and Drug Administration. A qualified health care professional should be consulted before using any therapeutic product discussed. All readers and continuing education participants should verify all information and data before treating patients or employing any therapies described in this continuing education activity.
Faculty
Jack Vinciguerra, PharmD
Freelance Medical Writer
East Hartford, CT
Faculty Disclosure
In accordance with the Accreditation Council for Pharmacy Education (ACPE) Criteria for Quality and Interpretive Guidelines, The University of Connecticut School of Pharmacy requires that faculty disclose any relationship that the faculty may have with commercial entities whose products or services may be mentioned in the activity.
Jack Vinciguerra has no relationships with ineligible companies.
ABSTRACT
Generic drug interchangeability is a key factor when verifying a prescription. Generic medications are essential in the modern American healthcare system, impacting patient care, medication access, and healthcare costs. However, this wasn’t always the case. Contributions over the past two centuries—including the publication of the first National Formulary in 1888, the development of early pharmaceutical standards by the pivotal 1938 Food, Drug, and Cosmetic Act, and the transformative 1984 Hatch-Waxman Act—have shaped today's definition of generic drugs. Over time, the U.S. Food and Drug Administration (FDA) has worked to strengthen and clarify the criteria for therapeutic equivalence, ensuring that generic drugs perform exactly like their brand-name counterparts. Additionally, specific approval pathways are established for brand-name drugs, standard generics, and authorized generics to ensure safety and market considerations are properly evaluated. The clinical implications of drug switching are emphasized, especially for narrow therapeutic index medications, where subtle variations require strict oversight. The practical application of the FDA's "Orange Book" for small-molecule generics and the "Purple Book" for biosimilars can help pharmacists make informed and legally sound substitutions that balance affordability, quality, and safety.
CONTENT
Content
INTRODUCTION
In modern pharmacy practice, the concept of generic drug interchangeability is crucial for patient care, medication accessibility, and healthcare expenses. Since pharmacists fill approximately 90% of prescriptions with generic drugs and biosimilars, they are essential in handling substitution challenges and ensuring therapeutic equivalence.1 Cost savings remain a primary motivation for switching to generics, which are among the few ways the United States (U.S.) healthcare system reduces overall spending.1 Nevertheless, safety must never be sacrificed for savings. Pharmacy employees and healthcare providers must understand the regulations, bioequivalence criteria, and clinical considerations related to interchangeable drugs, particularly when managing medications with narrow therapeutic indices.
THE GENERIC DRUG TIMELINE
The history of the generic drug industry is marked by challenges and controversies from its inception to the present day. Over the years, scrutiny and doubt have shaped what we recognize as generic drugs now.
So, what is a generic drug?
The Food and Drug Administration (FDA) defines a generic drug as a medication that is identical to a previously marketed brand-name drug in terms of dosage form, intended use, performance, quality, route of administration, safety, and strength. It functions exactly like the brand-name drug and offers the same clinical benefits, making it an equivalent substitute.2 However, brand-name and generic drugs have minor differences, discussed later.
In 1888, the American Pharmaceutical Association (now called the American Pharmacists Association, or APhA) published the first National Formulary (NF) to support the U.S. Pharmacopoeia (USP). The NF sets official standards for commonly used pharmaceutical preparations to help prevent counterfeit branded products.3 While not initially a legally recognized official document, it laid the foundation for the Roosevelt administration's passage of the Federal Pure Food and Drugs Act in 1906.4 This law banned adulterated or misbranded food and drugs for humans or animals, and allowed the government to hold companies accountable if a product caused serious harm. It also required drugs to meet standards of purity, quality, and potency established by the USP or NF—standards maintained by the FDA, formerly known as the Bureau of Chemistry.5
By the 1930s, the significant flaws in the Pure Food and Drug Act had become increasingly evident. Ingredient lists on products were optional, drug factory inspections lacked standardization, and there were no laws preventing unsafe products from reaching consumers. At that point, manufacturers could market and advertise drugs without substantial evidence of safety or effectiveness.5 Desperate to inform the public, the FDA compiled a collection of dangerous products legally available at the time. This exhibit, later called “The Chamber of Horrors,” debuted at the 1933 World’s Fair in Chicago and featured5,6
- Lash Lure, a popular cosmetic eyelash and eyebrow enhancer for women sold in many beauty salons, resulting in permanent blindness and disfigurement
- X-rays of children’s esophagi after ingesting candy with embedded trinkets, including coins, rings, or small lead toys*
- The Diana Ideal Womb Supporter, which could puncture the uterus if inserted incorrectly
*Table 1 describes the FDA’s stance on popular global treats.
Table 1. Surprise! FDA Cracks Down on Popular Treats7
| Kinder Surprise | Cracker Jack | |
| FDA STATUS | Banned in U.S. | Legal in U.S. |
| Why it’s banned/legal | Toy inside the chocolate egg violates FDCA, prohibits non-nutritive objects from being embedded in food.** | Toy packaged separately from food in the original box. FDA considers this “commingling,” not embedding, therefore is not a violation of the FDCA. |
| Safety Concern | The toy being directly inside the chocolate is considered a significant choking hazard for young children. | The FDA deems this to be safe because the toy is distinctly separate from the food itself. |
| ABBREVIATIONS: FDA, Food and Drug Administration; U.S., United States; FDCA, Food, Drug, and Cosmetics Act | ||
**In 2017, the U.S. version of Kinder Surprise, Kinder Joy, hit the market, consisting of an egg-shaped package that splits into two halves–one with chocolate, one with a small toy.
The critical watershed event occurred in October 1937.8 Earlier that year, scientists at the Pasteur Institute in France recognized sulfanilamide as a miracle drug for the treatment of streptococcal infections. Since the antibiotic was originally synthesized in 1908 and was no longer under patent (the legal right to be the sole producer or seller of a product), multiple pharmaceutical companies rushed to market it. One such company was S.E. Massengill. Their sales team noticed that sore throats, especially in children, were a common symptom of streptococcal infections. Seeing an opportunity, the company developed the first liquid form of the antibiotic, Elixir Sulfanilamide. They distributed 240 gallons of this mixture, containing 10% sulfanilamide, 16% water, and 72% diethylene glycol, across the U.S. without conducting toxicity tests. Of the 353 patients who used it, 105 died from acute kidney failure caused by diethylene glycol-induced proximal tubular necrosis.8 The FDA initiated a nationwide recall of any remaining Elixir Sulfanilamide. The government charged S.E. Massengill with selling a misbranded drug in interstate commerce. The elixir, not because of its toxic constituents, but because it lacked the required alcohol vehicle, was classified as illegal under current laws.5
Following arguably the most impactful mass poisonings of the 20th Century, Congress enacted the Food, Drug, and Cosmetic Act (FDCA) in June 1938. This law was a significant step forward in consumer protection and laid the groundwork for many of the public health improvements we see today. Under the FDCA, the FDA is tasked with several responsibilities9:
- Mandating drug manufacturers to submit safety data before marketing
- Setting quality standards for food, drugs, medical devices, and cosmetics
- Inspecting manufacturing and storage facilities
- Regulating labeling and claims for foods and dietary supplements
- Approving new drugs, medical devices, food, or color additives
While the FDCA significantly strengthened drug regulation in the U.S., it also created a new issue. Once a patent on a pioneering or brand-name drug expired, other companies could produce identical versions without needing to undergo the FDA’s strict safety and efficacy testing. These derivative (or generic) products, which vary in quality, then entered the market.4
Table 2 describes two significant amendments to the FDCA. Both continued the push towards stricter manufacturing expectations and categorical designations to achieve safe and effective administration of pharmaceuticals.10,11
Table 2. Amendments to the Food, Drug, and Cosmetic Act4,10,11
| Name of Amendment | Accomplishments | Downfalls |
| Durham-Humphrey Amendment of 1951 | · Created distinction of legend vs OTC pharmaceuticals
· Developed procedures for written, oral, and refilled prescriptions · Anti-substitution legislation often required pharmacists to dispense either the branded drug or a generic drug from a specific manufacturer, decreasing substitution of low-quality generics |
· Adequate manufacturers of generic products had limited opportunity due to anti-substitution laws and the public’s increased skepticism of generic drug quality
· Legend drugs now requiring a prescription from a licensed provider drastically cut the pharmacist’s role in selecting the most appropriate therapeutic option |
| Kefauver-Harris Amendments (1962) | · FDA now granted authority to require proof of efficacy in addition to safety before approval of a new drug
· A retrospective review of all drugs approved between 1938 and 1962 that let to nearly 600 ineffective medicines pulled off the market |
· New burden of evidence increased the cost and length of drug development, leading to a significant drug lag
· Indirectly led to the extension of drug patents in the Hatch-Waxman Act of 1984 |
| ABBREVIATIONS: OTC = over-the-counter; FDA = Food and Drug Administration | ||
Under the Kefauver-Harris Amendments, the requirements for new drug applications (NDA) diminished incentives to develop new generics. Generic manufacturers became frustrated because they had to invest considerable time and money in safety and efficacy studies that had already been completed for the brand-name drugs they sought to replicate. By 1983, only 35% of the top-selling branded medications with expired patents faced generic competition. Furthermore, pharmacists could only dispense a generic drug if it was explicitly prescribed.11
The Generic Drug Boom
The Drug Price Competition and Patent Term Restoration Act of 1984, known as the Hatch-Waxman Act (H-WA), transformed the generic drug industry.12 It sped up the approval process for generic drugs, establishing an Abbreviated NDA (ANDA) based solely on bioequivalence to the reference listed drug (brand-name). Once the FDA recognizes these generics as therapeutically equivalent, healthcare providers can regularly substitute them for prescriptions. It also allowed manufacturers to start testing before the brand’s patent expired, and the first successful ANDA filing would receive 180 days of market exclusivity after patent expiration. The H-WA also benefited and continues to help brand manufacturers by restoring patent time lost due to FDA testing, with a maximum extension of five years. Additionally, brand-name firms received three years of exclusivity for improvements resulting from clinical trials, such as new dosage forms, drug release methods, or dosage regimens. For example, Ambien CR (zolpidem tartrate extended-release tablets), was a widely used medication for insomnia. Its manufacturer updated Ambien’s immediate release mechanism by designing a dual-layered tablet where 50% of the drug releases immediately to help induce sleep, and the other 50% releases slowly to help maintain sleep.12
The H-WA immediately led to high financial risks, intense competition, and, unfortunately, widespread fraud.12 On the day the H-WA took effect, regulatory affairs members from Bolar Pharmaceuticals drove to the FDA headquarters and hand-delivered 40 ANDAs in an effort to secure the 180-day market exclusivity granted to the first successful generic drug applicant. Upon reviewing the submissions, the FDA discovered that all of Bolar’s submissions were fraudulent, having been fabricated solely to be the first company to file.12
The five years following the enactment of the H-WA became known as the "Generic Drug Scandal." An investigation by a government subcommittee revealed widespread bribery and numerous instances of fraudulent data submissions to the FDA. Only about six of 39 generic drug companies investigated avoided criminal or regulatory penalties.12 Public confidence in generic drugs dropped sharply, with a 1989 Gallup poll showing 51% of Americans doubted that generics met the same manufacturing standards as brand-name drugs. Recognizing the need for decisive action, the FDA responded with a series of reforms, including12
- Enactment of the Generic Drug Enforcement Act, allowing the FDA to take legal action against individuals or companies that violate FDA regulations
- Release of a comprehensive product analysis report reviewing 2500 samples from the 30 most prescribed generic drugs; less than 1% failed to meet standards
- Development of a strong application queue system within the Office of Generic Drugs, which included a pre-approval inspection process to verify the accuracy of data submitted with applications
- Requirement for all ANDAs to be complete upon submission. Drug manufacturers can no longer modify incomplete applications with additional data after they are filed
In the 21st Century, generic medications have remained a key part of the U.S. healthcare system. Congress has enacted several acts and amendments over the past 25 years to support and sustain the generic drug pathway (see Table 3). The FDA continues to promote the development of generic drugs by releasing a biannual list of drugs that have been off-patent for more than a year and have no generic competitors, and by establishing an expedited pathway for drugs designated as competitive generic therapies. This list can be found on the FDA’s website under “List of Off-Patent, Off-Exclusivity Drugs without an Approved Generic.”13
Table 3. Notable Updates to Generic Drug Regulations in the 21st Century13,14,15
| YEAR | NAME OF LEGISLATION | PURPOSE |
| 2003 | Medicare Prescription Drug, Improvement, and Modernization Act | Addressed loopholes used by brand-name companies to delay generic approval during patent litigation. |
| 2009 | Biologics Price Competition and Innovation Act | Developed the approval pathway for biosimilars (generic versions of complex biologic drugs) and appropriate “highly similar” standards because biologics cannot be perfectly replicated. |
| 2012 | Generic Drug User Fee Amendments | Requires generic drug companies to pay annual fees to expedite the FDAs review of generic applications. |
PAUSE AND PONDER: Given the historical context of drug regulation, how do you think public perception and trust in generic drugs today are influenced by past events like the Elixir Sulfanilamide tragedy or the Generic Drug Scandal, even with robust current regulations?
Approval Pathway of Drugs
Transforming a molecular compound into a well-known drug involves an extensive, expensive, and risky process. Usually, it takes 10 to 15 years and costs about $1 to $2 billion to approve a new drug, depending on the therapeutic area. Between 2010 and 2017, clinical trial data indicated a 90% failure rate among drug candidates that progressed to phase 1 testing. Including failed candidates in preclinical stages, the failure rate would be even higher.16
The initial stage of drug development is the preclinical phase. During this stage, a pharmaceutical company or research institution must demonstrate to the FDA that the drug candidate is reasonably safe for human trials.17 This involves a combination of in vitro (within a test tube or glass) and in vivo (within a living organism) studies that must establish six essential components18:
- Creation of drug substance/active pharmaceutical ingredient
- Dosage design (formulation)
- Analytical and bioanalytical method development and validation
- Metabolism and pharmacokinetics (PK)
- Toxicology and pharmacologic safety
- Current Good Manufacturing Practice (cGMP) and documentation of the drug candidate for use in clinical trials
At this point, a drug developer can submit an Investigational New Drug (IND) application to the FDA, which includes data from preclinical animal tests and the plan for human trials. The FDA and a local institutional review board (IRB)—comprising scientists and healthcare professionals from different institutions and hospitals involved in clinical research—review the application.17 An IRB must also approve a clinical trial protocol that includes17
- The study’s objectives and length
- Description of eligible trial participants
- Schedule of tests and procedures
- Medications and dosages used
- Participant consent
The clinical studies portion of drug development consists of four phases.19
Phase 1 focuses on the pharmacology and toxicity of the drug candidate. Absorption, distribution, metabolism, and excretion data help determine a safe and tolerable dose range for later trials. These trials typically involve small groups of subjects, often fewer than 20 healthy volunteers. Phase 1 is usually the shortest, lasting between nine and 18 months.19
Phase 2 evaluates the safety and effectiveness of the investigational drug. The clinical trials aim to determine how well the drug treats the target condition, helping to establish dosing regimens or parameters for future research. During this phase, the participant pool expands to hundreds of individuals with the condition under study, enabling the identification of other target populations and potential drug interactions. Typical studies at this stage are often blinded, randomized, controlled trials with specific inclusion and exclusion criteria. These studies usually last from one to three years.19
Phase 3 studies aim to confirm the drug’s therapeutic efficacy and benefit. Common questions considered in Phase 3 studies include19
- Can a dose-response relationship be established?
- Can the target population be increased?
- Can the drug be used at different stages of the disease?
- Can common side effects and food or drug interactions be identified?
Phase 3 also includes developing a product label with clear administration instructions. The study sample increases to about 1,000 subjects with the relevant condition, with minimal inclusion or exclusion criteria. This phase can last up to five years.19 Once finished, the drug company can formally submit its NDA to the FDA for approval. The FDA then has 60 days to either file the application for review or mark it incomplete if required data is missing. The Center for Drug Evaluation and Research (CDER) conducts the final NDA review. Under the Prescription Drug User Fee Act, CDER is expected to review and decide on at least 90% of NDAs for standard drugs within 10 months.17 The patent term of the brand drug is 20 years from the date the FDA files the NDA.20
Phase 4 trials are a post-marketing requirement of the FDA.17 These studies often highlight the difference between efficacy (which is a clinical trial’s construct) and effectiveness (which is how the drug performs in the real world). An investigational drug may be efficacious in the controlled environment of a Phase 2 trial, where strict inclusion criteria, constant monitoring, and perfect adherence are maintained. An effective drug performs without all of those guarantees.21 Real-world data collection for a newly approved drug often focuses on19
- Monitoring the drug safety profile, especially in populations not previously studied
- Identifying long-term adverse events
- Optimizing the application of the drug
- Determining potential contraindications in combination with other drugs or diseases
Post-approval trials may last up to three years or longer, as determined by the FDA.
After the brand-name patent expires and before a generic drug reaches pharmacy shelves, the FDA must conduct a comprehensive review of the product. Generic manufacturers must adhere to the same cGMP regulations as brand-name drug manufacturers, ensuring consistency, purity, and quality comparable to those of brand-name products across batches. These cGMP guidelines also enforce strict oversight of all manufacturing facilities.22 According to H-WA, approval of generics depends on demonstrating bioequivalence and pharmaceutical equivalence to the brand-name drug. Since generic developers do not need to repeat safety and effectiveness studies already conducted for the original drug, the ANDA was introduced.12 This simplified process means manufacturers only need to scientifically show that their drug performs similarly to the brand-name, without submitting new preclinical and clinical data.23 Table 4 provides a list of the data submission requirements for brand-name and generic drugs.
Table 4. Brand-Name Versus Generic Drug Data Submission Requirements23
| Brand-Name Requirements | Generic Requirements |
| Chemistry | Chemistry |
| Manufacturing | Manufacturing |
| Testing | Testing |
| Labeling | Labeling |
| Inspections | Inspections |
| Animal Studies | Bioequivalence |
| Clinical Studies | |
| Bioavailability |
SIDEBAR: “Can you tell me where my medication is from?”
If you've ever worked in a community pharmacy, chances are a customer asked about the source of their medication at least once. Although it might seem like a minor or unnecessary question, important reasons may prompt such inquiries.
Katherine Eban’s “Bottle of Lies: The Inside Story of the Generic Drug Boom,” a 2019 New York Times bestseller, reveals the dark side of some overseas generic medication manufacturing practices.
The story follows the journey of an ex-Ranbaxy (a generic drug company in India) employee turned whistleblower as he helps the FDA expose the poor operating standards of his former company. The protagonist witnessed multiple levels of deception and fraud, including24
- Intentional data falsification and manipulation
- Using a brand-name product to perform bioequivalence testing and publishing the results as data for the generic drug
- Unreported variations in generic drug effectiveness between batches
- Shipping drugs that did not meet the standards of one country to another country with less strict market standards.
Ranbaxy was not the only culprit; this was just the tip of the iceberg. Because the manufacturing sites of these generic drug companies were located on the opposite side of the world, the FDA couldn't investigate and monitor practices as frequently as it would for a company in the U.S. Additionally, the FDA would notify these companies weeks or even months in advance of a visit, giving the companies ample time to conceal their fabricated data and prepare their workers to provide the right lies to the FDA.24
Over time, evidence began to accumulate in the U.S.24 Many pharmacologists, doctors, and healthcare providers began noticing patterns in their patients’ reactions to certain generic drugs. Adverse reactions to generic narrow therapeutic index (NTI) drugs like levothyroxine and phenytoin started to rise. Doctors would try to switch patients to the generic version of their maintenance medication needed for managing chronic conditions, only to see those patients develop hyperthyroidism or experience an immediate uptick in seizures. Drugs with specially designed release profiles also came under scrutiny. Several patient complaints led Ted Cooperman, president of the independent laboratory ConsumerLab, to test Teva’s generic Budeprion XL against GSK’s brand-name Wellbutrin XL. The results were shocking – the generic drug released four times as much active ingredient in the first two hours as the brand-name did.24
Although some justice was achieved when Ranbaxy agreed to pay a $500 million settlement, the largest settlement to date with a generic drug manufacturer, the broader issue was fully revealed.24 When produced properly and in compliance with regulations, generic drugs positively impact medicine worldwide. Unfortunately, a certain level of vigilance is necessary, and pharmacy teams need to consider and report patient concerns when relevant. To stay informed, sign up on the FDA website to receive alerts about recalls, market withdrawals, and safety notices.
For a generic drug to be recognized as an adequate and appropriate substitution for a brand-name drug, the FDA formulated a simple equation25:
Pharmaceutical Equivalence (PE) + Bioequivalence (BE) = Therapeutic Equivalence (TE)
PE is demonstrated between two drug products if all of the following characteristics are identical25
- Dosage form
- Route(s) of administration
- Amount of active drug ingredient
- Amount of active drug ingredient delivered over a dosing period
- USP standard of drug identity, strength, quality, and purity
BE is entirely determined by what happens to a drug after it enters the body.26 There is a common misconception that a generic drug must contain 80% to 125% of the active ingredient present in the branded product to be considered bioequivalent. Equal doses of the active ingredient in both the generic and reference drugs must become available at the site of drug action at rates and extents that are not significantly different. The entire 90% confidence interval of PK measures, including area under the curve and peak concentration, must be between 0.80 and 1.25 to achieve BE. Determining BE through PK performance explains why differences in excipient content, color, or shape can occur between the generic and the reference listed drug.26
Only after demonstrating both PE and BE can a generic drug attain TE. As a TE product, the generic drug can then be included in the FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations list, commonly known as the "Orange Book." The generic drug now enjoys complete interchangeability with its brand-name counterpart.25, 27
Fun Fact: The FDA chose an orange cover for the first annual edition of the Approved Drug Products with Therapeutic Equivalence Evaluations List because it was published on Halloween in 1980. This festive choice led to the colloquial name, the "Orange Book," which has remained ever since.28
Authorized Generics
Imagine this situation: You are the CEO of PharmaZen Labs, a successful (fictitious) pharmaceutical company. Your flagship drug, ZenoLog, a fast-acting insulin, is about to lose its patent. Veta Pharmaceuticals, a generic drug producer, is eagerly waiting for the new year because the FDA has approved its ANDA for insulin-fastpart, the first generic version of ZenoLog. Veta plans to sell insulin-fastpart at a price 10 times lower than ZenoLog during the 180-day exclusivity period. The expected losses for ZenoLog in the upcoming year, due to competition from insulin-fastpart and other anticipated generics entering the market later, are considerable. You call for an urgent all-hands meeting to brainstorm ways to counter the bleak projections from the finance team. The room falls silent, tense and expectant. You glance around, hoping someone will have a solution. Suddenly, a tentative hand rises from a woman in the legal department. She quietly suggests, “What if we made our own generic?”
Congress was unprepared for a loophole in the H-WA: Authorized Generic (AG) drugs. In 1984, the idea that a brand-name company would produce a generic drug to compete with its own brand and first-market generic was unlikely.29 AGs refer to generic medications made by the same manufacturer as the brand-name product. They are identical in composition, shape, and size to the brand-name drug. Oftentimes, AGs and brand-name products are manufactured in the same facility.
In some cases, the AG may have a different marking or color. Standard generic drugs, however, often differ from the brand version in terms of shape, color, size, and inactive ingredients. AGs are a separate category of generics, and the FDA does not require their manufacturers to seek approval through the ANDA pathway because they are marketed under the brand-name NDA.30 Two significant distinctions evolved from this categorical differentiation of generic medicines29,30:
- AGs are excluded from the "Orange Book" because they fall under the proprietary NDA.
- An AG can directly compete with a standard generic during the 180-day exclusivity period because the law only prohibits other ANDA submissions. There is no restriction on launching identical versions of branded products through NDA supplementation.
In a community pharmacy setting, pharmacists and pharmacy technicians may dispense AGs frequently without realizing it. For example, Pfizer, a leading name in the pharmaceutical industry, developed Viagra in 1998. In 2003, Pfizer acquired Greenstone LLC, making it its generic subsidiary. The Viagra patent expired on December 11, 2017. On that day, Pfizer announced that Greenstone’s AG sildenafil was available alongside generic sildenafil from Teva Pharmaceuticals.31,32
AGs have recently ignited significant debate. In 2013, the Supreme Court recognized the financial significance of the 180-day exclusivity period for generic drug manufacturers, valuing it at hundreds of millions of dollars.33 From a consumer standpoint, the faster a drug's price drops substantially, the better, regardless of the manufacturer. A recent notable example of an AG is Mylan’s epinephrine auto-injector, the first generic of any kind for the EpiPen.33 Public and political outrage over Mylan’s 400% price hike for EpiPen accelerated the company’s decision to bring an affordable alternative to market. Other generic versions soon followed, helping to reduce costs and address supply chain issues often associated with the EpiPen.34
PAUSE AND PONDER: Considering the strategic move by brand-name companies to launch AGs to compete with their own products, what are the potential long-term implications for both generic manufacturers (especially smaller ones) and for overall drug pricing and patient access?
Narrow Therapeutic Index Drugs
Effective generic drugs have undoubtedly enhanced global healthcare by reducing costs, boosting competition, and increasing access to affordable medicines, thereby improving health outcomes.35 In most cases, TE products achieve their intended clinical effect even with minor variations in PK parameters compared to the brand-name versions. The FDA’s recommended BE range of 80% to 125% is suitable for most drugs, as the gap between the minimum therapeutic concentration and toxic levels is sufficiently large. This ensures the drug remains safe and clinically effective.36
The FDA defines NTIs as drugs with slight differences in dose or measured blood level that may result in therapeutic failure and/or potentially fatal adverse reactions. While the FDA does not maintain a formal list of NTIs, as of January 2024, it has updated the product-specific considerations for 14 active ingredients for prospective generic drug manufacturers (see Table 5).37
Table 5. Examples of Drugs with Narrow Therapeutic Indexes37,38
| DRUG CATEGORY | EXAMPLES |
| Anticoagulants | Warfarin*, Heparin |
| Antiepileptics | Valproic Acid*, Phenobarbital*, Phenytoin*, Carbamazepine* |
| Aminoglycosides | Streptomycin, Kanamycin, Netilmicin, Tobramycin, Neomycin |
| Immunosuppressants | Cyclosporine*, Sirolimus*, Everolimus*, Tacrolimus*, Mycophenolic Acid |
| Glycosides | Digoxin* |
| Mood-stabilizers | Lithium carbonate* |
| Thyroid Agents | Levothyroxine*, Liothyronine* |
| Bronchodilator | Theophylline* |
*FDA indicated the product as NTI in product-specific consideration provided to generic drug manufacturers
PAUSE AND PONDER: For NTIs, where subtle variations can have significant clinical consequences, how might pharmacists and healthcare providers best navigate the balance between cost savings through generic substitution and ensuring optimal patient safety and efficacy?
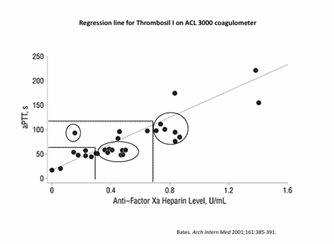
BE studies in healthy individuals often show similar average exposure between generic and brand-name drugs, but this does not ensure TE for every patient, especially with sensitive drug classes like antiepileptics or cardiovascular medications. This is crucial because average BE studies, which measure mean differences, may not account for individual patient variability in PK, risking underdosing or overdosing in some cases.39 PK variability within the same patient, rather than the quality of generics themselves, has been identified as a key factor in adverse drug reactions after switching medications.40
Although two generics may be bioequivalent to the brand-name drug, the FDA does not explicitly approve them as interchangeable. For example, variations in excipients—often considered inert—can significantly impact drug bioavailability and cause substantial differences in BE, as seen with alendronate, where certain excipients of a generic product increased bioavailability by 5-fold compared to Fosamax.41 The American Academy of Neurology has also expressed concern about generic substitution in antiepileptic therapy. The organization has recommended prioritizing brand-name treatments and opposing a generic switch without prescriber approval.42 A recent study also pointed out that the nocebo effect (adverse effects that occur just because the patient believes they may occur) can reduce patient adherence when a generic is substituted for a brand-name medication. Patients may feel that the medication is less effective or experience more adverse effects, even if there is no actual pharmacologic difference induced.43,44
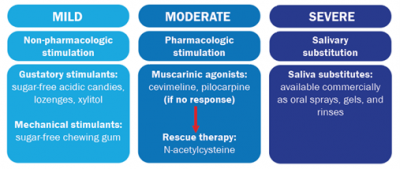
The FDA continues to work on mitigating the adverse effects of NTIs. In 2015, they formed the NTI Drug Working Group to develop a consistent approach for NTI classification and transparently address and resolve current issues.37 The Working Group also aims to standardize methodologies for assessing BE, including shrinking the conventional 80% to 125% limits or implementing a scaled average BE approach that adjusts limits based on the reference-listed drug's within-subject variability.45 For example, the BE of levothyroxine has been tightened to 90% to 110% to account and critical dose-response. The FDA has implemented strict updates to cGMP, increasing oversight of excipient selection, formulation stability, and dissolution profiles. This proactive approach helps safeguard patient safety by ensuring that every stage of drug manufacturing—from sourcing raw materials to releasing the final product—adheres to the highest quality control and process validation standards.46 Post-market surveillance and risk management programs designed explicitly for NTIs continuously monitor safety events. Adverse event reporting systems, combined with pharmacoepidemiologic studies and real-world data analysis, track emerging safety concerns or subtherapeutic performance.47 The FDA also often requires a Risk Evaluation and Mitigation Strategies (REMS) program for NTIs, which includes clear and comprehensive product labeling, specialized medication guides, and proactive communication plans for medical emergencies.48
The Orange Book
The "Orange Book" serves as a comprehensive guide for identifying drug products that the FDA considers therapeutically equivalent. It facilitates the substitution of brand-name medications with their generic counterparts.49 The FDA’s division of Orange Book Publication and Regulatory Assessment within the Office of Generic Drugs updates the text monthly to ensure accurate and up-to-date information.50 This equivalence is confirmed when generic drugs contain the same active ingredients, dosage form, strength, route of administration, and labeling as their brand-name equivalents, eliminating the need for repeated phase 1, 2, and 3 clinical trials. 51 The Orange Book thus supports state laws on generic substitution, allowing pharmacists to dispense therapeutically equivalent generic options, which greatly contributes to cost savings for both consumers and state healthcare systems.52 This approach aligns with public health goals by increasing access to affordable medications while ensuring safety and efficacy.53,54
Despite its usefulness, relying solely on the Orange Book for interchangeability has limitations, especially in assessing BE for complex drug products and accounting for the diversity of state regulations that may influence substitution practices.55 For example, some states permit therapeutic substitution, where a pharmacist can replace a prescribed drug with a chemically different but therapeutically similar alternative without prior approval. This differs from generic substitution, which requires that the drug be bioequivalent and pharmaceutically equivalent, ensuring the generic performs identically to the brand-name drug in the body.50 The TE ratings listed in the book further illustrate the differences among approved products. The two-letter code associated with the drug product differentiates between TE and PE products. The coding system also indicates if a product has corrected previously identified BE issues. Table 6 provides an in-depth description of the coding system.56
Table 6. TE Coding System56
| RATING | DESCRIPTION |
| AA | Therapeutically equivalent to other therapeutically equivalent products with no history of BE issues |
| AB | Previous BE issue resolved with adequate in vivo/in vitro data, product is BE to Reference Listed Drug |
| AA/AN/AO/AP/AT | No in vivo BE issue identified, second letter indicates dosage form (i.e., O = injectable, N = aerosolized solutions/powders) |
| B | Not therapeutically equivalent to other pharmaceutically equivalent products |
| BC/BD/BE/BN/BP/BR/BS/BT/BX/B* | Drug products of specific formulation that have unresolved BE issues (i.e., BR: suppositories or enemas for systemic use, B*: drug products requiring further investigation and review) |
| NR | Not rated (i.e., authorized generics) |
| NA | Products not reviewed by FDA (i.e., vitamins, supplements) |
| Off-market | Off-market – includes TE code when product went off the market |
| ABBREVIATIONS: BE = bioequivalence; FDA = Food and Drug Administration; TE = therapeutic equivalence | |
State regulations vary from mandatory substitution laws—where pharmacists must replace a drug with a less expensive generic unless the prescriber specifies otherwise—to permissive laws that allow but do not mandate substitution.57 Some states also include therapeutic substitution policies, broadening the scope beyond bioequivalent generics to incorporate chemically different but clinically similar alternatives when approved by a physician. These diverse legal frameworks highlight the complex landscape of pharmaceutical dispensing, which is often shaped by state-specific views on safety, effectiveness, and cost control.50
The Purple Book
The Purple Book, officially known as "Lists of Licensed Biological Products with Reference Product Exclusivity and Biosimilarity or Interchangeability Evaluations," operates similarly to the Orange Book but is specific to biologics. It provides guidance on substituting original biologics with their biosimilar and interchangeable biosimilar versions. This is crucial because biologic products, due to their complex manufacturing processes and natural variability, cannot be classified as standard generics like small-molecule drugs.54 Unlike chemically-made small-molecule drugs, biologics come from living organisms, making exact replication impossible and necessitating a different regulatory approach for approval and interchangeability.58 Consequently, the FDA has implemented strict criteria for biosimilarity, requiring comprehensive analytical, animal, and clinical data to demonstrate that a biosimilar is highly similar to the reference product, with no meaningful differences in safety, purity, and potency.59 The Purple Book plays an essential role in promoting the development and accessibility of more affordable biologic products by identifying those that meet these high standards for biosimilarity and interchangeability.60 This extensive resource supports healthcare providers and patients in making informed choices about biologic substitutions, intending to foster market competition and reduce healthcare costs for expensive biological therapies, which have historically lacked generic alternatives.
CONCLUSION
The journey of generic drugs, from initial regulatory challenges to their current indispensable role, underscores a continuous effort to balance medication accessibility, cost-effectiveness, and patient safety in healthcare.1,4 We've seen how pivotal events, such as the Elixir Sulfanilamide tragedy and the subsequent FDCA of 1938, laid the foundation for robust drug regulation, which was further refined by amendments like the Durham-Humphrey and Kefauver-Harris Acts.5,10,11
The landscape of generic drug approval was dramatically reshaped by the H-WA of 1984, which streamlined the ANDA process and significantly boosted generic competition.12 While this led to an initial "generic drug boom," it also highlighted the need for stringent oversight, prompting reforms like the Generic Drug Enforcement Act following the Generic Drug Scandal.12
Crucially, the concept of TE, established through PE and BE, ensures that generic drugs perform identically to their brand-name counterparts, providing the same clinical benefits.2, 25 Resources like the Orange Book for small-molecule drugs and the Purple Book for biologics are essential guides for identifying therapeutically equivalent products, facilitating safe and effective substitutions.49, 60 However, the complexities associated with NTI drugs and the emergence of AGs demonstrate that vigilance and continuous regulatory adaptation are paramount to maintaining public trust and optimizing patient outcomes.29,36
As approximately 90% of prescriptions are filled with generics and biosimilars, pharmacists, pharmacy technicians, and healthcare providers play a critical role in navigating these complexities.1 The ongoing evolution of regulations, particularly around NTIs and biosimilars, reflects the commitment to ensuring that cost savings do not compromise the safety and efficacy of essential medications. Ultimately, the robust regulatory framework surrounding generic drugs aims to provide patients with access to affordable, high-quality treatments, reinforcing their status as a cornerstone of modern healthcare.
Finally, readers may be wondering about the Green Book, referenced in the title. The Green Book is the FDA’s List of Approved Animal Drug Products!
Pharmacist Post Test (for viewing only)
LAW: Orange, Purple, Green Books: Learning Generics' True Colors
25-074 Pharmacist Post-test
After completing this continuing education activity, pharmacists will be able to
• Review the regulatory timeline of generic drugs in the United States.
• Define the regulatory and scientific criteria for therapeutic equivalence, including bioequivalence and pharmaceutical equivalence, as established by the U.S. Food and Drug Administration (FDA).
• Differentiate between brand-name, generic, and authorized generic drug products, identifying key differences in composition, cost, and approval pathways.
• Discuss the clinical implications of switching between drug products, especially those with a narrow therapeutic index (NTI).
• Apply state-specific laws and the FDA's "Orange Book" and “Purple Book” to make appropriate and legally sound generic substitutions.
1. Pharmacists are discussing the historical context of drug regulation with a new intern. They mention a pivotal event in 1937 that led to the enactment of the Food, Drug, and Cosmetic Act in 1938. What was this event, and what was its primary impact on drug regulation?
A. The publication of the first National Formulary, which banned manufacturers from selling adulterated products.
B. The Elixir Sulfanilamide tragedy, which mandated drug manufacturers to submit safety data before marketing.
C. The "Chamber of Horrors" exhibit, which led to the creation of over-the-counter drug classifications.
*
2. Following the Generic Drug Scandal in the late 1980s, public confidence in generic drugs significantly declined. To address this, the FDA implemented several reforms. Which of the following was a key reform aimed at restoring trust and ensuring drug quality?
A. Creating the "Orange Book" to assess therapeutic equivalence and guide recommended substitutions.
B. Enacting the Generic Drug Enforcement Act, allowing legal action against companies violating regulations.
C. Requiring all new drugs to undergo extensive clinical trials in three phases, including generics.
*
3. A pharmacist is evaluating two drug products that both contain 10 mg of atorvastatin calcium, are in tablet form, and are administered orally. To determine if these two products are pharmaceutically equivalent, what additional characteristic must be identical?
A. The bioavailability of the active ingredient.
B. The rate and extent to which the active ingredient is absorbed into the bloodstream.
C. The compendial standard of drug identity, strength, quality, and purity.
*
4. The FDA has just approved a new generic version of a commonly prescribed antidepressant. For this generic to be considered bioequivalent to the brand-name product, what are the primary measures that must fall within the 80% to 125% range relative to the reference drug?
A. Physical measures like the size and the color of the tablet.
B. Maximal drug potency and receptor occupancy.
C. AUC and peak concentration of active drug in the body.
*
5. A brand-name pharmaceutical company's patent for its blockbuster drug has expired. To maintain market share, the company decides to release an "Authorized Generic" version of its own drug. How does this AG differ from a standard generic in terms of its approval pathway?
A. The AG must undergo a complete Abbreviated New Drug Application process like a standard generic.
B. The AG is marketed under the brand-name drug's existing New Drug Application and does not require a separate ANDA.
C. The AG completes the AG-Mini Application and is directly listed in the "Orange Book" with an 'AB' rating.
*
6. During a pharmacy consultation, a patient is excited to learn that the expensive brand-name medication she has taken for years now has a standard generic option available. The patient is concerned that if the pill looks different, it cannot be the same medication. How should a pharmacist explain the difference between brand-name and standard generic medications in terms of appearance and inactive ingredients?
A. Tell the patient not to worry; standard generics must be identical in shape, color, and inactive ingredients to the brand-name drug for bioequivalence.
B. Explain to the patient that standard generics often vary in shape, color, and inactive ingredients from the brand but still maintain therapeutic equivalence.
C. Let the patient know that even if the color and shape might be a little different, you are pretty sure all the ingredients should be the same.
*
7. A new generic drug has received 180 days of market exclusivity after being the first successful ANDA filing post-patent expiration. However, a few weeks later, the brand-name company launches its own Authorized Generic. What is the implication of the Authorized Generic's entry during this exclusivity period?
A. The Authorized Generic can directly compete with the standard generic because the law only prohibits other ANDA submissions.
B. The Authorized Generic is prohibited from competing during the 180-day exclusivity period while the manufacturer submits an ANDA.
C. The FDA will immediately revoke the 180-day exclusivity period for the standard generic due to the AG's launch.
*
8. A patient with epilepsy who has been stable on Dilantin is switched to a generic phenytoin by their insurance company to reduce costs. Phenytoin is known to be a Narrow Therapeutic Index drug. What is a key clinical consideration for the pharmacist and prescriber in this situation?
A. The patient may experience a nocebo effect, or even actual therapeutic failure or toxicity due to subtle pharmacokinetic variations.
B. Minor variations in excipients are always insignificant for NTI drugs, and this patient’s response will eventually even out.
C. Generic substitution is always safe for NTI drugs because the FDA ensures identical performance of ALL generic drugs.
*
9. A pharmacist is trying to find an interchangeable biologic for a patient's prescribed biologic. Which FDA publication should the pharmacist consult for guidance on biosimilars and interchangeable biosimilars?
A. The Orange Book
B. The Purple Book
C. The National Formulary
*
10. A pharmacist in a state with "mandatory substitution laws" receives a prescription for a brand-name drug for which therapeutically equivalent generics are available. Unless specifically indicated by the prescriber, what action is the pharmacist legally required to take?
A. Replace the brand-name drug with a less expensive therapeutically equivalent generic.
B. Substitute the brand-name drug with a chemically different but therapeutically similar alternative.
C. Dispense the prescribed brand-name medication because that is what the physician ordered.
Pharmacy Technician Post Test (for viewing only)
LAW: Orange, Purple, Green Books: Learning Generics' True Colors
25-074 Technician Post-test
After completing this continuing education activity, pharmacists will be able to
• Review the regulatory timeline of generic drugs in the United States.
• Define the regulatory and scientific criteria for therapeutic equivalence, including bioequivalence and pharmaceutical equivalence, as established by the U.S. Food and Drug Administration (FDA).
• Differentiate between brand-name, generic, and authorized generic drug products, identifying key differences in composition, cost, and approval pathways.
• Discuss the clinical implications of switching between drug products, especially those with a narrow therapeutic index (NTI).
• Apply state-specific laws and the FDA's "Orange Book" and “Purple Book” to make appropriate and legally sound generic substitutions.
1. Pharmacists are discussing the historical context of drug regulation with a new intern. They mention a pivotal event in 1937 that led to the enactment of the Food, Drug, and Cosmetic Act in 1938. What was this event, and what was its primary impact on drug regulation?
A. The publication of the first National Formulary, which banned manufacturers from selling adulterated products.
B. The Elixir Sulfanilamide tragedy, which mandated drug manufacturers to submit safety data before marketing.
C. The "Chamber of Horrors" exhibit, which led to the creation of over-the-counter drug classifications.
*
2. Following the Generic Drug Scandal in the late 1980s, public confidence in generic drugs significantly declined. To address this, the FDA implemented several reforms. Which of the following was a key reform aimed at restoring trust and ensuring drug quality?
A. Creating the "Orange Book" to assess therapeutic equivalence and guide recommended substitutions.
B. Enacting the Generic Drug Enforcement Act, allowing legal action against companies violating regulations.
C. Requiring all new drugs to undergo extensive clinical trials in three phases, including generics.
*
3. A pharmacist is evaluating two drug products that both contain 10 mg of atorvastatin calcium, are in tablet form, and are administered orally. To determine if these two products are pharmaceutically equivalent, what additional characteristic must be identical?
A. The bioavailability of the active ingredient.
B. The rate and extent to which the active ingredient is absorbed into the bloodstream.
C. The compendial standard of drug identity, strength, quality, and purity.
*
4. A patient picks up a prescription and notices his generic medication looks identical in shape, size, and color to the brand-name drug he used to take, even though the manufacturer’s name is different. The patient asks the pharmacy technician why this is. What is the most accurate explanation?
A. This generic is likely an Authorized Generic and is manufactured by the same company as the brand-name drug, often making it identical in appearance.
B. All generic drugs are required to look exactly like their brand-name counterparts, so this is normal and expected.
C. The pharmacy received and dispensed a mislabeled product; the patient should return the prescription and report it as required by state law.
*
5. A brand-name pharmaceutical company's patent for its blockbuster drug has expired. To maintain market share, the company decides to release an "Authorized Generic" version of its own drug. How does this AG differ from a standard generic in terms of its approval pathway?
A. The AG must undergo a complete Abbreviated New Drug Application process like a standard generic.
B. The AG is marketed under the brand-name drug's existing New Drug Application and does not require a separate ANDA.
C. The AG completes the AG-Mini Application and is directly listed in the "Orange Book" with an 'AB' rating.
*
6. During a pharmacy consultation, a patient is excited to learn that the expensive brand-name medication she has taken for years now has a standard generic option available. The patient is concerned that if the pill looks different, it cannot be the same medication. How should a pharmacist explain the difference between brand-name and standard generic medications in terms of appearance and inactive ingredients?
A. Tell the patient not to worry; standard generics must be identical in shape, color, and inactive ingredients to the brand-name drug for bioequivalence.
B. Explain to the patient that standard generics often vary in shape, color, and inactive ingredients from the brand but still maintain therapeutic equivalence.
C. Let the patient know that even if the color and shape might be a little different, you are pretty sure all the ingredients should be the same.
*
7. A new generic drug has received 180 days of market exclusivity after being the first successful ANDA filing post-patent expiration. However, a few weeks later, the brand-name company launches its own Authorized Generic. What is the implication of the Authorized Generic's entry during this exclusivity period?
A. The Authorized Generic can directly compete with the standard generic because the law only prohibits other ANDA submissions.
B. The Authorized Generic is prohibited from competing during the 180-day exclusivity period while the manufacturer submits an ANDA.
C. The FDA will immediately revoke the 180-day exclusivity period for the standard generic due to the AG's launch.
*
8. A patient with epilepsy who has been stable on Dilantin is switched to a generic phenytoin by their insurance company to reduce costs. Phenytoin is known to be a Narrow Therapeutic Index drug. What is a key clinical consideration for the pharmacist and prescriber in this situation?
A. The patient may experience a nocebo effect, or even actual therapeutic failure or toxicity due to subtle pharmacokinetic variations.
B. Minor variations in excipients are always insignificant for NTI drugs, and this patient’s response will eventually even out.
C. Generic substitution is always safe for NTI drugs because the FDA ensures identical performance of ALL generic drugs.
*
9. A pharmacist is trying to find an interchangeable biologic for a patient's prescribed biologic. Which FDA publication should the pharmacist consult for guidance on biosimilars and interchangeable biosimilars?
A. The Orange Book
B. The Purple Book
C. The National Formulary
*
10. A pharmacist in a state with "mandatory substitution laws" receives a prescription for a brand-name drug for which therapeutically equivalent generics are available. Unless specifically indicated by the prescriber, what action is the pharmacist legally required to take?
A. Replace the brand-name drug with a less expensive therapeutically equivalent generic.
B. Substitute the brand-name drug with a chemically different but therapeutically similar alternative.
C. Dispense the prescribed brand-name medication because that is what the physician ordered.
References
Full List of References
1. Murphy J. 2025 Generic and Biosimilar Medicines Savings Report Highlights Value and Vulnerability. Association for Accessible Medicines. Published September 5, 2025. Accessed September 19, 2025. https://accessiblemeds.org/resources/blog/2025-generic-and-biosimilar-medi
2. Generic Drugs: Questions & Answers. Food and Drug Administration; March 2021. Accessed September 20, 2025. https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/generic-drugs-questions-answerscines-savings-report-highlights-value-and-vulnerability/
3. McCarthy R. EVOLUTION OF THE PHARMACOPOEIA. aihp.org. Spring 2016. Accessed September 20, 2025.
4. Hornecker JR. Generic Drugs: History, Approval Process, and Current Challenges. US Pharm. 2009;34(6)(Generic Drug Review suppl):26-30. https://www.uspharmacist.com/article/generic-drugs-history-approval-process-and-current-challenges. Accessed September 19, 2025.
5. Swann JP. How Chemists Pushed for Consumer Protection: The Food and Drugs Act of 1906. Chem Herit. 2006;24(2):6-11. https://digital.sciencehistory.org/works/jdtfjzq/viewer/slnr4t2#q=1906. Accessed September 20, 2025.
6. Public Outreach Remains Powerful Agency Tool. Food and Drug Administration; March 2023. Accessed November 6, 2025. https://www.fda.gov/about-fda/regulatory-news-stories-and-features/public-outreach-remains-powerful-agency-tool
7. Johnson J. When Cracker Jack had to Throw out the Toy. FDA Storytime. Published October 6, 2017. Accessed November 16, 2025. https://fdastorytime.com/2017/10/06/when-cracker-jacks-had-to-throw-out-the-toy/
8. Paine MF. Therapeutic disasters that hastened safety testing of new drugs. Clin Pharmacol Ther. 2017;101(4):430-434. doi:10.1002/cpt.613
9. Lam C, Patel P. Food, Drug, and Cosmetic Act. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 31, 2023. Accessed October 4, 2025.
10. Kleiman MA, Hawdon JE. Durham-Humphrey Act. Encyclopedia of Drug Policy. Vol. 2. Thousand Oaks, CA: SAGE Publications, Inc.; 2011: 264-265. doi:10.4135/9781412976961.n112
11. Greene JA, Podolsky SH. Reform, regulation, and pharmaceuticals--the Kefauver-Harris Amendments at 50. N Engl J Med. 2012;367(16):1481-1483. doi:10.1056/NEJMp1210007
12. Boehm G, Yao L, Han L, Zheng Q. Development of the generic drug industry in the US after the Hatch-Waxman Act of 1984. Acta Pharmaceutica Sinica B. 2013;3(5):297-311. doi:10.1016/j.apsb.2013.07.004
13. Competitive Generic Therapies. Food and Drug Administration. October 2022. Accessed October 18, 2025. https://www.fda.gov/media/136063/download
14. Koyfman H. Biosimilarity and Interchangeability in the Biologics Price Competition and Innovation Act of 2009 and FDA's 2012 Draft Guidance for Industry. Biotechnol Law Rep. 2013;32(4):238-251. doi:10.1089/blr.2013.9884
15. Berndt ER, Conti RM, Murphy SJ. The generic drug user fee amendments: an economic perspective. J Law Biosci. 2018;5(1):103-141. Published 2018 Apr 11. doi:10.1093/jlb/lsy002
16. Sun D, Gao W, Hu H, Zhou S. Why 90% of clinical drug development fails and how to improve it? Acta Pharmaceutica Sinica B. 2022;12(7):3049-3062. doi:10.1016/j.apsb.2022.02.002
17. The FDA’s Drug Review Process: Ensuring Drugs Are Safe and Effective. Food and Drug Administration; November 2017. Accessed October 19, 2025. https://www.fda.gov/drugs/information-consumers-and-patients-drugs/fdas-drug-review-process-ensuring-drugs-are-safe-and-effective
18. Steinmetz KL, Spack EG. The basics of preclinical drug development for neurodegenerative disease indications. BMC Neurol. 2009;9(Suppl 1). doi:10.1186/1471-2377-9-s1-s2
19. The four phases of clinical trials. acrpnet.org. June 2016. Accessed October 20, 2025. https://acrpnet.org/wp-content/uploads/dlm_uploads/2016/10/The-Four-Phases-of-Clinical-Trials_June-2016-1.pdf
20. Frequently Asked Questions of Patents and Exclusivity. Food and Drug Administration; February 2020. Accessed October 20, 2025. https://www.fda.gov/drugs/development-approval-process-drugs/frequently-asked-questions-patents-and-exclusivity#howlongpatentterm
21. Suvarna V. Phase IV of Drug Development. Perspect Clin Res. 2010;1(2):57-60.
22. Terrie Y. A Review of First-Time Generic Drug Approvals. US Pharm. 2024;49(6):35-40. Accessed October 19, 2025. https://www.uspharmacist.com/article/a-review-of-firsttime-generic-drug-approvals
23. Terrie Y. Parsing the Generic-Drug Approval Process. US Pharm. 2018;43(6):10-16. Accessed October 19, 2025. https://www.uspharmacist.com/article/parsing-the-genericdrug-approval-process
24. Eban K. Bottle of Lies: The inside Story of the Generic Drug Boom. Ecco, an imprint of HarperCollins Publishers; 2020.
25. Myung J. Introduction of Bioequivalence for Generic Drug Products. Lecture presented at Regulatory Best Practices for Global Access to Medicines, Including Anti-TB Medicines Conference. August 18, 2022; Virtual Presentation.
26. Andrade C. Bioequivalence of generic drugs: A simple explanation for a US Food and Drug Administration Requirement. J Clin Psychiatry. 2015;76(06):e742-e744. doi:10.4088/jcp.15f10094
27. Zhu H, Zhou H, Seitz K. Chapter 15 - Bioavailability and Bioequivalence. In: Developing Solid Oral Dosage Forms: Pharmaceutical Theory And Practice. Academic Press; 2009:341-364.
28. Canterbury C, Nguyen K, Coogan A. Freshly Squeezed: Orange Book History and Key Updates at 45. FDLI Update Magazine. Published online May 20, 2025. Accessed November 16, 2025. https://www.fdli.org/2025/05/freshly-squeezed-orange-book-history-and-key-updates-at-45/#_ednref27
29. Hamer M, Rose A. Authorized Generics: To Switch Rather than Fight. GEN Biotechnol. 2005;25(13). Accessed October 20, 2025. https://www.genengnews.com/news/authorized-generics-to-switch-rather-than-fight/
30. Alderfer J. Authorized Generics: What Pharmacists Should Know. US Pharm. 2020;45(6):23. Accessed October 20, 2025. https://www.uspharmacist.com/article/authorized-generics-what-pharmacists-should-know
31. Johnson L. Drugmaker launches own generic Viagra. Times Union. https://www.timesunion.com/business/article/Drugmaker-launches-own-generic-Viagra-12418747.php. Published December 9, 2017. Accessed October 22, 2025.
32. Teva announces exclusive launch of generic Viagra® Tablets in the United States. tevapharm.com. December 11, 2017. Accessed October 22, 2025. https://www.tevapharm.com/news-and-media/latest-news/teva-announces-exclusive-launch-of-generic-viagra-tablets-in-the-united-states/
33. Fowler AC, Jacobo-Rubio R, Xu J. Authorized generics in the US: Prevalence, characteristics, and timing, 2010–19. Health Aff (Millwood). 2023;42(8):1071-1080. doi:10.1377/hlthaff.2022.01677
34. Brennan Z. Authorized generics: Why Mylan would compete with itself in the epipen market. Regulatory Affairs Professional Society. August 29, 2016. Accessed November 20, 2025. https://www.raps.org/News-and-Articles/News-Articles/2016/8/Authorized-Generics-Why-Mylan-Would-Compete-With
35. The U.S. Generic & Biosimilar Medicines Savings Report. accessiblemeds.org. 2018. Accessed October 23, 2025. https://accessiblemeds.org/wp-content/uploads/2025/01/AAM-2024-Generic-Biosimilar-Medicines-Savings-Report.pdf.
36. Tamargo J, Le Heuzey JY, Mabo P. Narrow therapeutic index drugs: a clinical pharmacological consideration to flecainide. Eur J Clin Pharmacol. 2015;71(5):549-567. doi:10.1007/s00228-015-1832-0
37. Donnelly M, Fang L, Madabushi R, et al. Narrow Therapeutic Index Drugs: FDA Experience, Views, and Operations. Clin Pharmacol Ther. 2025;117(1):116-129. doi:10.1002/cpt.3460
38. Gozzo L, Caraci F, Drago F. Bioequivalence, Drugs with Narrow Therapeutic Index and The Phenomenon of Biocreep: A Critical Analysis of the System for Generic Substitution. Healthcare (Basel). 2022;10(8):1392. Published 2022 Jul 26. doi:10.3390/healthcare10081392
39. Glerum PJ, Neef C, Burger DM, Yu Y, Maliepaard M. Pharmacokinetics and Generic Drug Switching: A Regulator's View. Clin Pharmacokinet. 2020;59(9):1065-1069. doi:10.1007/s40262-020-00909-8
40. Chen M, Chow SC. Assessing bioequivalence and drug interchangeability. J Biopharm Stat. 2017;27(2):272-281. doi:10.1080/10543406.2016.1265537
41. Zarmpi P, Flanagan T, Meehan E, Mann J, Østergaard J, Fotaki N. Biopharmaceutical implications of excipient variability on drug dissolution from immediate release products. Eur J Pharm Biopharm. 2020;154:195-209. doi:10.1016/j.ejpb.2020.07.014
42. Rahman MM, Alatawi Y, Cheng N, et al. Comparison of brand versus generic antiepileptic drug adverse event reporting rates in the U.S. Food and Drug Administration Adverse Event Reporting System (FAERS). Epilepsy Res. 2017;135:71-78. doi:10.1016/j.eplepsyres.2017.06.007
43. Kristensen LE, Alten R, Puig L, et al. Non-pharmacological Effects in Switching Medication: The Nocebo Effect in Switching from Originator to Biosimilar Agent. BioDrugs. 2018;32(5):397. doi:10.1007/s40259-018-0306-1
44. Giron NC, Oh H, Rehmet E, Shireman TI. Descriptive Trends in Medicaid Antipsychotic Prescription Claims and Expenditures, 2016 - 2021. J Behav Health Serv Res. 2024;51(4):516-528. doi:10.1007/s11414-024-09889-0
45. Jiang W, Makhlouf F, Schuirmann DJ, et al. A Bioequivalence Approach for Generic Narrow Therapeutic Index Drugs: Evaluation of the Reference-Scaled Approach and Variability Comparison Criterion. AAPS J. 2015;17(4):891-901. doi:10.1208/s12248-015-9753-5
46. Concordet D, Gandia P, Montastruc JL, et al. Why Were More Than 200 Subjects Required to Demonstrate the Bioequivalence of a New Formulation of Levothyroxine with an Old One?. Clin Pharmacokinet. 2020;59(1):1-5. doi:10.1007/s40262-019-00812-x
47. Diak IL, Swank K, McCartan K, et al. The Food and Drug Administration’s (FDA’s) Drug Safety Surveillance During the COVID-19 Pandemic. Drug Saf. 2023;46(2):145. doi:10.1007/s40264-022-01256-2
48. Dąbrowska A. FDA Risk Evaluation and Mitigation Strategies (REMS): Description and Effect on Generic Drug Development. Published online April 11, 2017. Accessed November 16, 2025. https://sgp.fas.org/crs/misc/R44810.pdf
49. Song Y, Barthold D. The effects of state‐level pharmacist regulations on generic substitution of prescription drugs. Health Econ. 2018;27(11):1717. doi:10.1002/hec.3796
50. Socal MP, Cordeiro T, Anderson GF, Bai G. Estimating Savings Opportunities from Therapeutic Substitutions of High-Cost Generic Medications. JAMA Netw Open. 2022;5(11). doi:10.1001/jamanetworkopen.2022.39868
51. Kesselheim AS, Gagne JJ. Product-Specific Regulatory Pathways to Approve Generic Drugs: The Need for Follow-up Studies to Ensure Safety and Effectiveness. Drug Saf. 2015;38(10):849. doi:10.1007/s40264-015-0315-7
52. Mishuk AU, Fasina I, Qian J. Impact of U.S. federal and state generic drug policies on drug use, spending, and patient outcomes: A systematic review. Res Social Adm Pharm. 2020;16(6):736-745. doi:10.1016/j.sapharm.2019.08.031
53. Howard JN, Harris I, Frank G, Kiptanui Z, Qian J, Hansen R. Influencers of generic drug utilization: A systematic review. Res Social Adm Pharm. 2018;14(7):619-627. doi:10.1016/j.sapharm.2017.08.001
54. Dunne S, Shannon B, Dunne C, Cullen W. A review of the differences and similarities between generic drugs and their originator counterparts, including economic benefits associated with usage of generic medicines, using Ireland as a case study. BMC Pharmacol Toxicol. 2013;14:1. Published 2013 Jan 5. doi:10.1186/2050-6511-14-1
55. Tam A, Garcia-Arieta A, Abalos I, et al. A Survey of the Criteria Used for the Selection of Alternative Comparator Products by Participating Regulators and Organizations of the International Pharmaceutical Regulators Programme. J Pharm Pharm Sci. 2022;25:323-339. doi:10.18433/jpps33081
56. Manigault K, Marcheva G, Peasah S. Insights into Effective Generic Substitution. US Pharm. Published online June 16, 2016. Accessed October 20, 2025. https://www.uspharmacist.com/article/insights-into-effective-generic-substitution.
57. Nakipov Z, Musaev U, Smagylova I, et al. Validation of Kazakh and Russian Generic Drug Questionnaire. Med J Islam Repub Iran. 2025;39:101. Published 2025 Jul 30. doi:10.47176/mjiri.39.101
58. Walsh G, Walsh E. Biopharmaceutical benchmarks 2022. Nat Biotechnol. 2022;40(12):1722-1760. doi:10.1038/s41587-022-01582-x
59. Evans C, Gibofsky A, Strand V. Biosimilars for immune-mediated inflammatory diseases: a managed care perspective. Am J Manag Care. 2022;28(12 Suppl):S234-S239. doi:10.37765/ajmc.2022.89298
60. Dusetzina SB, Keating NL, Huskamp HA, Mello MM. Medicare’s Plan for Drug-Price Negotiation — The Importance of Defining Generic Entry. N Engl J Med. 2023;389(2):97. doi:10.1056/nejmp2304289